Epilepsy is a neurological disorder characterized by recurrent, unprovoked seizures caused by abnormal electrical activity in the brain. Effective management often involves medications, lifestyle adjustments, and sometimes surgical interventions to control and reduce seizure frequency. Discover essential insights into epilepsy treatment, symptoms, and support options in the rest of this article.
Table of Comparison
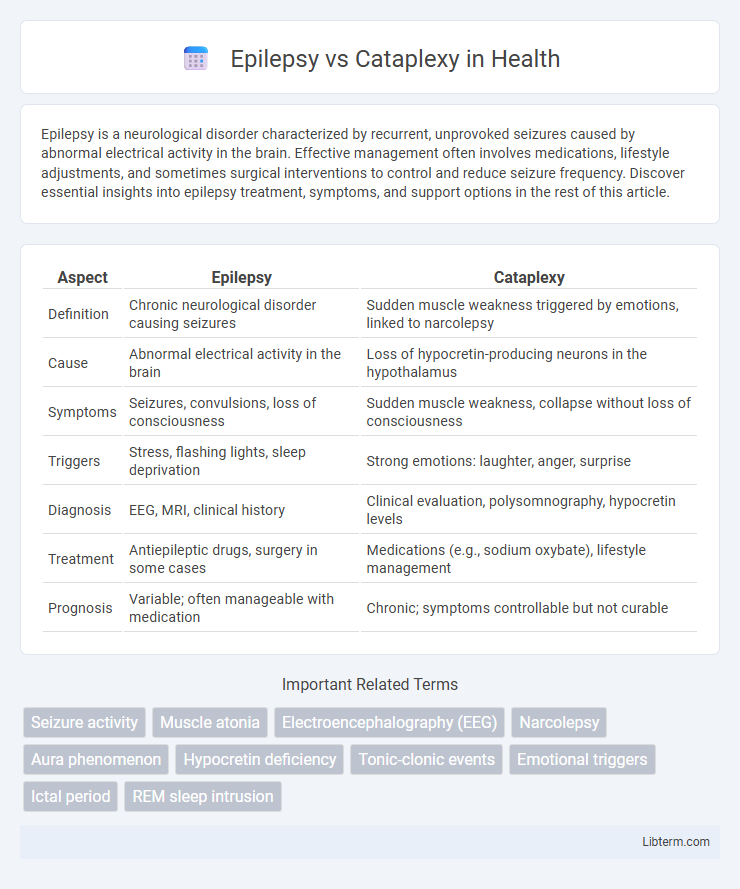
| Aspect | Epilepsy | Cataplexy |
|---|---|---|
| Definition | Chronic neurological disorder causing seizures | Sudden muscle weakness triggered by emotions, linked to narcolepsy |
| Cause | Abnormal electrical activity in the brain | Loss of hypocretin-producing neurons in the hypothalamus |
| Symptoms | Seizures, convulsions, loss of consciousness | Sudden muscle weakness, collapse without loss of consciousness |
| Triggers | Stress, flashing lights, sleep deprivation | Strong emotions: laughter, anger, surprise |
| Diagnosis | EEG, MRI, clinical history | Clinical evaluation, polysomnography, hypocretin levels |
| Treatment | Antiepileptic drugs, surgery in some cases | Medications (e.g., sodium oxybate), lifestyle management |
| Prognosis | Variable; often manageable with medication | Chronic; symptoms controllable but not curable |
Introduction to Epilepsy and Cataplexy
Epilepsy is a neurological disorder characterized by recurrent, unprovoked seizures resulting from abnormal electrical activity in the brain. Cataplexy is a sudden, brief loss of muscle tone often triggered by strong emotions, commonly associated with narcolepsy, a sleep disorder. Understanding the distinct mechanisms and symptoms of epilepsy and cataplexy is essential for accurate diagnosis and appropriate treatment strategies.
Defining Epilepsy: Causes and Symptoms
Epilepsy is a neurological disorder characterized by recurrent, unprovoked seizures resulting from abnormal electrical activity in the brain. Causes include genetic factors, head trauma, brain infections, stroke, and tumors, while symptoms vary from convulsions and loss of consciousness to sensory disturbances and muscle spasms. Understanding the diverse manifestations and underlying causes is essential for differentiating epilepsy from conditions like cataplexy, which involves sudden muscle weakness triggered by strong emotions.
Understanding Cataplexy: Triggers and Manifestations
Cataplexy is characterized by sudden, brief episodes of muscle weakness or paralysis triggered by strong emotions such as laughter, surprise, or anger, distinguishing it from epilepsy, which involves abnormal brain electrical activity and seizures. Unlike epileptic seizures that can cause convulsions or loss of consciousness, cataplexy episodes typically preserve awareness while causing muscle collapse or weakness. Recognizing emotional triggers and the presence of muscle atonia during cataplexy is crucial for accurate diagnosis and effective management in patients with narcolepsy type 1.
Key Differences Between Epilepsy and Cataplexy
Epilepsy is characterized by recurrent, unprovoked seizures caused by abnormal electrical activity in the brain, whereas cataplexy involves sudden muscle weakness triggered by strong emotions, without loss of consciousness. Epileptic seizures can manifest with convulsions, sensory disturbances, or impaired awareness, while cataplexy episodes typically present as brief, reversible episodes of muscle atonia while the person remains fully conscious. Diagnosis relies on EEG findings for epilepsy and clinical history linked to narcolepsy for cataplexy.
Neurological Mechanisms: Epilepsy vs Cataplexy
Epilepsy involves abnormal, excessive electrical discharges in the brain's neurons leading to seizures, originating primarily from cortical hyperexcitability. Cataplexy results from sudden, transient loss of muscle tone triggered by emotional stimuli, linked to dysfunction in hypothalamic neurons producing hypocretin (orexin), which regulates wakefulness and muscle control. The key neurological distinction lies in epilepsy's hyperexcitable cortical networks versus cataplexy's hypothalamic hypocretin deficiency causing REM sleep intrusion into wakefulness.
Diagnosis: How Epilepsy and Cataplexy Are Identified
Epilepsy is diagnosed through electroencephalogram (EEG) tests that detect abnormal brain wave patterns and neuroimaging such as MRI to identify structural brain abnormalities. Cataplexy diagnosis relies on clinical evaluation of sudden muscle weakness triggered by strong emotions, often supported by polysomnography and multiple sleep latency tests (MSLT) to confirm narcolepsy. Distinguishing between epilepsy and cataplexy involves correlating patient history with diagnostic findings since EEG abnormalities are absent in cataplexy but common in epileptic seizures.
Common Misconceptions and Overlapping Symptoms
Epilepsy and cataplexy are frequently confused due to overlapping symptoms such as sudden loss of muscle control and brief episodes of altered consciousness, yet epilepsy involves abnormal electrical brain activity causing seizures, while cataplexy is a sudden, temporary muscle weakness triggered by strong emotions. Common misconceptions include mistaking cataplexy episodes for epileptic seizures, leading to misdiagnosis and inappropriate treatment. Accurate diagnosis requires comprehensive neurological evaluation and monitoring to distinguish epileptic seizures from cataplexy episodes triggered by narcolepsy.
Treatment Options: Managing Epilepsy and Cataplexy
Treatment options for epilepsy primarily include antiepileptic drugs (AEDs) like valproate, lamotrigine, and levetiracetam, which aim to reduce or eliminate seizure activity. Cataplexy management often involves medications such as sodium oxybate and antidepressants like selective serotonin reuptake inhibitors (SSRIs) or tricyclic antidepressants that help control sudden muscle weakness episodes. Both conditions benefit from individualized treatment plans, lifestyle adjustments, and regular monitoring to optimize symptom control and improve quality of life.
Living with Epilepsy or Cataplexy: Quality of Life
Living with epilepsy or cataplexy significantly impacts quality of life due to unpredictable episodes that disrupt daily routines and social interactions. Managing these conditions requires consistent medication adherence, lifestyle adjustments, and support systems to reduce seizure frequency and cataplexy attacks. Mental health challenges, including anxiety and depression, are common and necessitate integrated care approaches to improve overall well-being.
When to Seek Medical Help: Warning Signs and First Aid
Severe or prolonged seizures lasting more than five minutes, recurrent seizures without regaining consciousness, or sudden onset of muscle weakness triggered by strong emotions indicate the need for immediate medical attention in epilepsy and cataplexy. First aid for epilepsy includes protecting the person from injury, placing them in a recovery position, and calling emergency services if the seizure persists or breathing is impaired. In cataplexy, medical help is essential when episodes occur unexpectedly, causing falls or injuries, and treatments focusing on underlying narcolepsy should be pursued.
Epilepsy Infographic
 libterm.com
libterm.com