Insulinoma and adrenal adenoma are distinct types of tumors affecting different glands, with insulinoma originating in the pancreas and causing excessive insulin production, while adrenal adenoma arises in the adrenal glands and may impact hormone levels. Both conditions can result in significant metabolic disturbances requiring precise diagnosis and treatment. Discover more about their symptoms, diagnosis, and management strategies in the rest of this article.
Table of Comparison
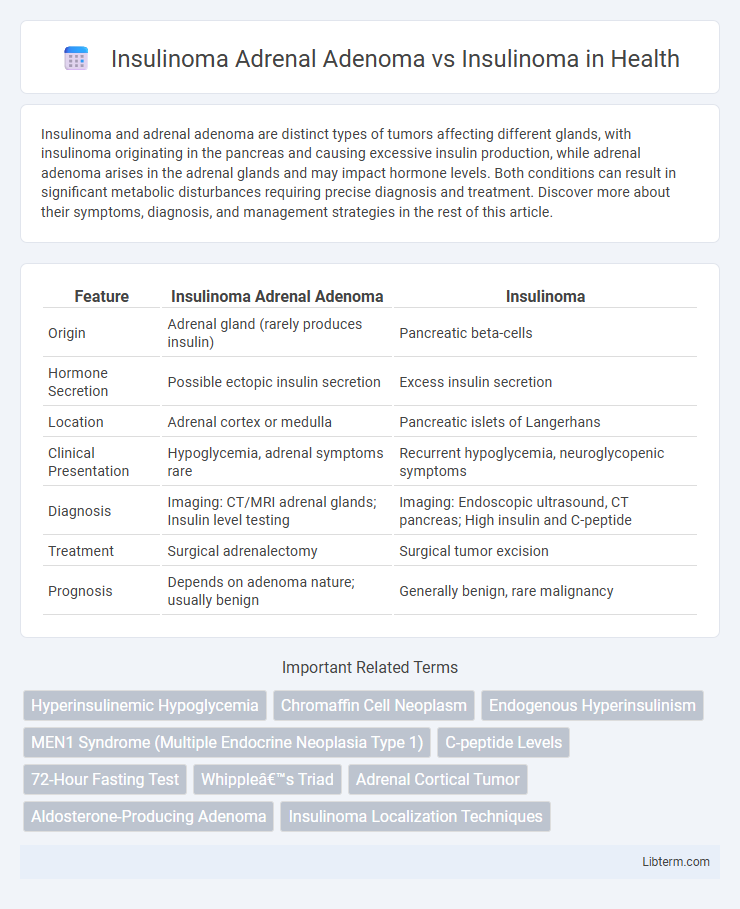
| Feature | Insulinoma Adrenal Adenoma | Insulinoma |
|---|---|---|
| Origin | Adrenal gland (rarely produces insulin) | Pancreatic beta-cells |
| Hormone Secretion | Possible ectopic insulin secretion | Excess insulin secretion |
| Location | Adrenal cortex or medulla | Pancreatic islets of Langerhans |
| Clinical Presentation | Hypoglycemia, adrenal symptoms rare | Recurrent hypoglycemia, neuroglycopenic symptoms |
| Diagnosis | Imaging: CT/MRI adrenal glands; Insulin level testing | Imaging: Endoscopic ultrasound, CT pancreas; High insulin and C-peptide |
| Treatment | Surgical adrenalectomy | Surgical tumor excision |
| Prognosis | Depends on adenoma nature; usually benign | Generally benign, rare malignancy |
Overview of Insulinoma and Adrenal Adenoma
Insulinoma is a rare pancreatic neuroendocrine tumor that secretes excessive insulin, leading to recurrent hypoglycemia and symptoms such as sweating, confusion, and palpitations. Adrenal adenoma is a benign tumor of the adrenal cortex that may be nonfunctional or produce hormones like cortisol, aldosterone, or androgens, causing conditions such as Cushing's syndrome or primary aldosteronism. Differentiating between insulinoma and adrenal adenoma involves biochemical tests, imaging studies like CT or MRI, and hormone level assessments to identify the tumor's origin and specific hormonal activity.
Causes and Pathophysiology
Insulinoma is a pancreatic beta-cell tumor causing increased insulin secretion, resulting in hypoglycemia. Insulinoma adrenal adenoma is a rare ectopic presentation where an adrenal adenoma aberrantly produces insulin, mimicking pancreatic insulinoma effects. Pathophysiologically, pancreatic insulinomas arise from islet cell hyperplasia or neoplasia, while adrenal insulin-producing adenomas involve ectopic beta-cell differentiation within adrenal cortical tissue.
Epidemiology and Risk Factors
Insulinomas are rare pancreatic neuroendocrine tumors with an incidence of 1-4 cases per million annually, primarily affecting adults aged 40-60 years, with no significant gender predilection. Adrenal adenomas, often incidental findings, occur in approximately 1-5% of the general population, increasing in prevalence with age and metabolic risk factors such as obesity and hypertension. Insulinoma adrenal adenoma coexistence is extremely rare, with limited epidemiological data, but metabolic syndrome and genetic syndromes like Multiple Endocrine Neoplasia type 1 (MEN1) may increase risk.
Clinical Presentation: Insulinoma vs Adrenal Adenoma
Insulinomas primarily present with symptoms of hypoglycemia such as confusion, sweating, and palpitations due to excessive insulin secretion. Adrenal adenomas, often incidental findings, may manifest with signs of hormone excess like hypertension or Cushing's syndrome, depending on hormone production. Unlike insulinomas, adrenal adenomas rarely cause hypoglycemia but can cause systemic effects related to cortisol or aldosterone overproduction.
Diagnostic Criteria and Approaches
Insulinoma adrenal adenoma and insulinoma differentiate primarily through imaging and biochemical testing, with insulinoma typically presenting as a pancreatic beta-cell tumor causing endogenous hyperinsulinemic hypoglycemia. Diagnostic criteria for insulinoma include a supervised 72-hour fast demonstrating Whipple's triad alongside elevated insulin, C-peptide, and proinsulin levels during hypoglycemia, while adrenal adenomas are often incidentalomas found on CT or MRI without endogenous insulin secretion. Localization techniques such as endoscopic ultrasound, somatostatin receptor scintigraphy, and selective arterial calcium stimulation testing aid in distinguishing pancreatic insulinomas from non-insulin-secreting adrenal adenomas.
Biochemical Markers and Laboratory Findings
Insulinoma adrenal adenoma and insulinoma differ significantly in biochemical markers and laboratory findings; insulinomas typically present with elevated insulin, C-peptide, and proinsulin levels during hypoglycemic episodes, confirming endogenous hyperinsulinemia. In contrast, adrenal adenomas usually do not secrete insulin but may affect cortisol and aldosterone levels, requiring differentiation through hormonal assays and imaging. Laboratory evaluation for insulinoma includes supervised fasting tests and measurement of plasma glucose, insulin, C-peptide, and proinsulin, whereas adrenal adenoma diagnosis involves adrenal hormone panels, including cortisol, aldosterone, and plasma renin activity.
Imaging Techniques for Detection
Insulinoma detection relies heavily on advanced imaging techniques such as endoscopic ultrasound (EUS) and contrast-enhanced CT scans, which provide high sensitivity for identifying small pancreatic lesions. Adrenal adenomas, although rare in the context of insulin secretion, are primarily evaluated using MRI and adrenal CT imaging to differentiate benign from malignant masses based on size, density, and washout characteristics. Combining functional imaging modalities like PET with radiotracers such as 68Ga-DOTATATE can improve localization accuracy and distinction between insulinoma and adrenal adenoma sources of hyperinsulinemic hypoglycemia.
Treatment Options and Management Strategies
Insulinoma Adrenal Adenoma requires a tailored management approach combining surgical resection of the adrenal gland tumor with medical therapy to control hypoglycemia, whereas insulinomas primarily demand focused enucleation or partial pancreatectomy. Preoperative stabilization through diazoxide or octreotide is common in both conditions to manage insulin-induced hypoglycemia. Postoperative monitoring and potential adjunctive therapies differ due to the distinct hormonal profiles and tumor locations, necessitating personalized endocrinologic assessment.
Prognosis and Long-term Outcomes
Insulinoma adrenal adenoma, a rare functional tumor arising from adrenal cortical cells with ectopic insulin production, generally demonstrates a favorable prognosis with surgical resection leading to resolution of hypoglycemia and low recurrence rates. In contrast, insulinoma originating from pancreatic beta cells often has excellent long-term outcomes post-resection but carries a slightly higher risk of malignancy and metastasis, necessitating close follow-up. Both conditions require biochemical monitoring and imaging surveillance, yet insulinoma adrenal adenoma's prognosis hinges on precise diagnosis due to its atypical presentation and potential for mismanagement.
Key Differences Between Adrenal Adenoma and Insulinoma
Insulinoma primarily originates from pancreatic beta cells causing hyperinsulinemic hypoglycemia, while adrenal adenomas are benign tumors of the adrenal cortex often producing steroids without insulin secretion. Key differences include anatomical location, with insulinomas found in the pancreas and adrenal adenomas in adrenal glands, and their hormonal activity--insulinomas secrete excess insulin, whereas adrenal adenomas may secrete cortisol or aldosterone. Diagnostic imaging and biochemical tests, such as insulin levels for insulinoma and serum cortisol or aldosterone for adrenal adenoma, are crucial to differentiate these entities.
Insulinoma Adrenal Adenoma Infographic
 libterm.com
libterm.com