Sepsis is a life-threatening condition that arises when the body's response to infection causes widespread inflammation leading to tissue damage. Early recognition and prompt treatment are crucial for improving survival rates and reducing complications. Discover more about the symptoms, causes, and treatments to protect your health in the full article.
Table of Comparison
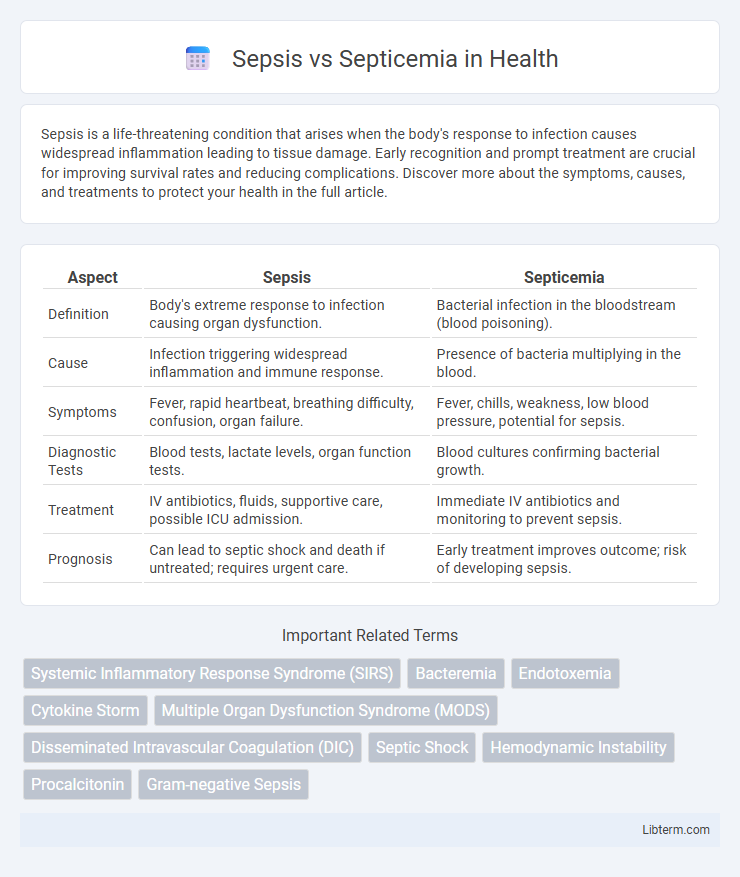
| Aspect | Sepsis | Septicemia |
|---|---|---|
| Definition | Body's extreme response to infection causing organ dysfunction. | Bacterial infection in the bloodstream (blood poisoning). |
| Cause | Infection triggering widespread inflammation and immune response. | Presence of bacteria multiplying in the blood. |
| Symptoms | Fever, rapid heartbeat, breathing difficulty, confusion, organ failure. | Fever, chills, weakness, low blood pressure, potential for sepsis. |
| Diagnostic Tests | Blood tests, lactate levels, organ function tests. | Blood cultures confirming bacterial growth. |
| Treatment | IV antibiotics, fluids, supportive care, possible ICU admission. | Immediate IV antibiotics and monitoring to prevent sepsis. |
| Prognosis | Can lead to septic shock and death if untreated; requires urgent care. | Early treatment improves outcome; risk of developing sepsis. |
Understanding Sepsis and Septicemia
Sepsis is a life-threatening condition that arises when the body's response to infection causes widespread inflammation, potentially leading to organ failure. Septicemia, often referred to as blood poisoning, specifically denotes the presence of bacteria in the blood causing sepsis but is sometimes used interchangeably with sepsis in clinical contexts. Recognizing the difference between sepsis as a systemic inflammatory response and septicemia as a bloodstream infection is crucial for timely diagnosis and treatment.
Definitions: Sepsis vs Septicemia
Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to infection, whereas septicemia specifically refers to the presence of bacteria in the bloodstream, also known as blood poisoning. Sepsis involves a complex immune response leading to widespread inflammation and potential multi-organ failure, while septicemia denotes the bloodstream infection itself that can lead to sepsis if untreated. Understanding the distinction is crucial for accurate diagnosis and timely management of these critical conditions.
Causes and Risk Factors
Sepsis results from the body's extreme response to an infection, commonly triggered by bacterial, fungal, or viral pathogens invading the bloodstream, tissues, or organs. Septicemia, specifically referring to the presence of bacteria in the blood, often originates from infections like pneumonia, urinary tract infections, or wounds that allow bacteria to enter the circulatory system. Risk factors for both conditions include weakened immune systems, chronic illnesses such as diabetes or cancer, recent surgeries or invasive procedures, and advanced age, which increase susceptibility to severe infections and systemic inflammatory responses.
Pathophysiology: How Sepsis and Septicemia Develop
Sepsis develops as a systemic inflammatory response triggered by an infection that leads to widespread immune activation and organ dysfunction. Septicemia specifically refers to the presence of pathogenic bacteria or their toxins in the bloodstream, causing a bloodstream infection that can progress to sepsis. The pathophysiology of septicemia involves bacterial proliferation in the blood, endotoxin release, and activation of the host immune system, which can escalate into sepsis if dysregulated.
Signs and Symptoms Comparison
Sepsis presents with signs such as fever, rapid heart rate, rapid breathing, confusion, and extreme pain or discomfort, indicating a systemic inflammatory response to infection. Septicemia, often referred to as blood poisoning, typically causes symptoms like chills, high fever, rapid breathing, and low blood pressure due to the presence of bacteria or their toxins in the bloodstream. While both conditions share symptoms like fever and rapid heart rate, septicemia specifically highlights bloodstream infection markers, whereas sepsis encompasses the broader immune response affecting multiple organ systems.
Diagnostic Criteria and Testing
Sepsis is diagnosed based on clinical criteria such as the Sequential Organ Failure Assessment (SOFA) score, which assesses organ dysfunction, and may include biomarkers like procalcitonin and lactate levels to evaluate infection severity. Septicemia, often used interchangeably with bloodstream infection or bacteremia, is confirmed through positive blood cultures identifying pathogenic microorganisms in the blood. Diagnostic testing for sepsis involves blood cultures, complete blood counts, and inflammatory markers, while septicemia diagnosis relies heavily on blood culture results to detect the presence of bacteria or fungi causing systemic infection.
Treatment Approaches for Sepsis and Septicemia
Treatment approaches for sepsis prioritize rapid administration of intravenous antibiotics and aggressive fluid resuscitation to stabilize blood pressure and support organ function. Septicemia treatment similarly involves prompt antibiotic therapy targeting the underlying bloodstream infection, alongside measures to prevent complications such as disseminated intravascular coagulation. Both conditions require careful monitoring in an intensive care setting with supportive therapies including vasopressors and oxygen supplementation to improve patient outcomes.
Complications and Prognosis
Sepsis often leads to life-threatening complications such as multi-organ failure, acute respiratory distress syndrome (ARDS), and disseminated intravascular coagulation (DIC), significantly worsening the prognosis. Septicemia, characterized by the presence of bacteria in the bloodstream, can rapidly progress to sepsis if untreated, increasing risks of septic shock and irreversible tissue damage. Early detection and prompt antibiotic therapy improve survival rates, yet both conditions carry high mortality risks without immediate medical intervention.
Prevention and Early Detection
Sepsis and septicemia prevention relies heavily on timely vaccination, proper wound care, and strict hygiene practices to reduce infection risks. Early detection involves monitoring for systemic inflammatory response syndrome (SIRS) signs such as fever, elevated heart rate, and rapid breathing, combined with blood culture tests to identify bloodstream infections. Prompt antibiotic administration and supportive care within the first hour of symptom onset significantly improve patient outcomes and reduce mortality rates.
Key Differences and Summary
Sepsis is a life-threatening organ dysfunction caused by a dysregulated host response to infection, whereas septicemia specifically refers to the presence of bacteria in the bloodstream (bacteremia) that leads to systemic infection. Key differences highlight that septicemia is a subset of sepsis, primarily indicating bloodstream infection, while sepsis encompasses a broader range of immune responses causing tissue damage and organ failure. Early recognition and treatment of sepsis are critical due to its rapid progression and high mortality, whereas septicemia diagnosis focuses on blood culture results confirming bacterial invasion.
Sepsis Infographic
 libterm.com
libterm.com