Antifungal treatments target fungal infections by inhibiting the growth and spread of fungi on skin, nails, or internal organs. These medications come in various forms, including creams, ointments, and oral tablets, tailored to the specific type and severity of the infection. Discover effective antifungal solutions and how to protect your health by reading the full article.
Table of Comparison
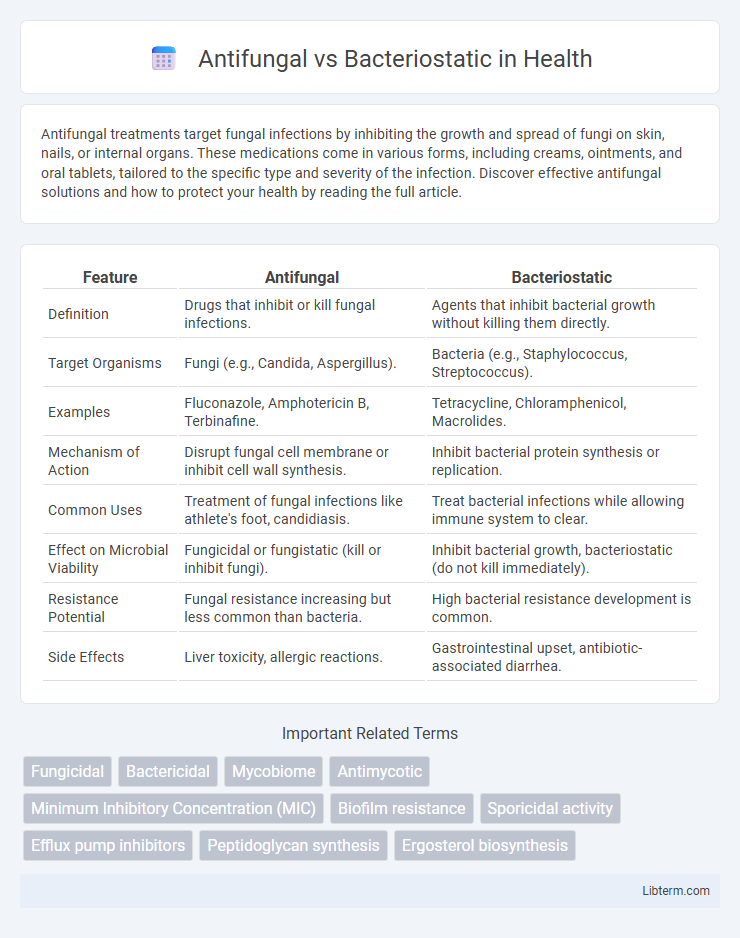
| Feature | Antifungal | Bacteriostatic |
|---|---|---|
| Definition | Drugs that inhibit or kill fungal infections. | Agents that inhibit bacterial growth without killing them directly. |
| Target Organisms | Fungi (e.g., Candida, Aspergillus). | Bacteria (e.g., Staphylococcus, Streptococcus). |
| Examples | Fluconazole, Amphotericin B, Terbinafine. | Tetracycline, Chloramphenicol, Macrolides. |
| Mechanism of Action | Disrupt fungal cell membrane or inhibit cell wall synthesis. | Inhibit bacterial protein synthesis or replication. |
| Common Uses | Treatment of fungal infections like athlete's foot, candidiasis. | Treat bacterial infections while allowing immune system to clear. |
| Effect on Microbial Viability | Fungicidal or fungistatic (kill or inhibit fungi). | Inhibit bacterial growth, bacteriostatic (do not kill immediately). |
| Resistance Potential | Fungal resistance increasing but less common than bacteria. | High bacterial resistance development is common. |
| Side Effects | Liver toxicity, allergic reactions. | Gastrointestinal upset, antibiotic-associated diarrhea. |
Understanding Antifungal and Bacteriostatic Agents
Antifungal agents target fungal cells by disrupting their cell membranes or interfering with critical enzymes, effectively treating fungal infections. Bacteriostatic agents inhibit bacterial growth and reproduction without directly killing the bacteria, allowing the immune system to eliminate the pathogens. Understanding the distinct mechanisms of antifungal and bacteriostatic agents is crucial for selecting appropriate treatments in managing infections caused by fungi and bacteria.
Key Differences: Antifungal vs Bacteriostatic Mechanisms
Antifungal agents target fungal cells by disrupting their cell membranes or inhibiting essential components like ergosterol, effectively killing or inhibiting fungal growth. Bacteriostatic agents inhibit bacterial proliferation by interfering with protein synthesis or metabolic pathways without directly killing the bacteria, allowing the immune system to eliminate the infection. The key difference lies in their mechanisms: antifungals directly damage fungal cell structures, while bacteriostatics primarily halt bacterial reproduction.
Types of Infections Treated by Antifungal and Bacteriostatic Drugs
Antifungal drugs primarily treat fungal infections such as candidiasis, aspergillosis, and dermatophytosis, targeting pathogens like Candida, Aspergillus, and dermatophytes. Bacteriostatic agents inhibit bacterial growth and are effective against infections caused by bacteria like Streptococcus, Staphylococcus, and Escherichia coli, commonly used in respiratory, urinary tract, and skin infections. Understanding the specific microbial targets and infection types is crucial for selecting appropriate antifungal or bacteriostatic therapies.
Common Antifungal Medications: Uses and Effects
Common antifungal medications such as fluconazole, itraconazole, and terbinafine effectively target fungal infections by inhibiting fungal cell membrane synthesis and disrupting cell growth. These agents are primarily used to treat conditions like athlete's foot, ringworm, and candidiasis, providing relief by eliminating the fungal pathogens responsible for infection. Unlike bacteriostatic drugs that inhibit bacterial growth without killing bacteria, antifungals actively destroy or neutralize fungal cells to control and eradicate fungal diseases.
Popular Bacteriostatic Agents: Applications and Limitations
Popular bacteriostatic agents such as tetracyclines, sulfonamides, and macrolides inhibit bacterial growth by interfering with protein synthesis or metabolic pathways, making them effective in treating various bacterial infections. Their applications range from respiratory tract infections to acne treatment, but their limitations include potential resistance development and reduced efficacy in immunocompromised patients. Understanding these constraints is crucial for optimizing therapy and preventing misuse in clinical practice.
Spectrum of Activity: Fungi vs Bacteria Targeting
Antifungal agents specifically target fungi by disrupting cell membrane integrity or inhibiting fungal enzyme systems, effectively treating infections like candidiasis and aspergillosis. Bacteriostatic drugs inhibit bacterial growth and reproduction without killing the bacteria directly, making them effective against a broad range of gram-positive and gram-negative bacteria. Understanding the distinct spectrum of activity is critical for selecting appropriate treatments, as antifungals are ineffective against bacteria and bacteriostatic agents have no impact on fungal pathogens.
Resistance Issues in Antifungal and Bacteriostatic Therapy
Resistance issues in antifungal therapy are increasingly problematic due to the adaptive mechanisms of fungi such as efflux pump overexpression and biofilm formation, reducing drug efficacy. Bacteriostatic agents face resistance challenges primarily through genetic mutations and horizontal gene transfer that alter target sites or induce efflux mechanisms. Understanding these resistance pathways is critical for developing effective treatment regimens and mitigating the rise of multidrug-resistant fungal and bacterial strains.
Side Effects and Safety Profiles Compared
Antifungal medications often cause side effects such as liver toxicity, gastrointestinal upset, and allergic reactions, whereas bacteriostatic agents typically present milder side effects including gastrointestinal disturbances and potential allergic responses. Safety profiles of antifungals require monitoring of liver enzymes due to their hepatotoxic potential, while bacteriostatic drugs generally have a wider therapeutic index and lower risk of serious toxicity. Both classes of drugs demand careful patient assessment to mitigate adverse effects, especially in individuals with pre-existing conditions or those taking multiple medications.
Clinical Scenarios: When to Choose Antifungal or Bacteriostatic Treatments
In clinical scenarios involving fungal infections such as candidiasis or dermatophytosis, antifungal treatments are essential to target and eradicate pathogenic fungi by disrupting their cell membranes or inhibiting ergosterol synthesis. Bacteriostatic agents are preferred in bacterial infections where halting bacterial proliferation allows the immune system to effectively clear the pathogen, as seen in mild to moderate infections caused by Streptococcus or Staphylococcus species. Selecting antifungal versus bacteriostatic therapy hinges on accurate diagnosis and pathogen identification to optimize treatment efficacy and avoid resistance.
Future Advances in Antimicrobial Therapy
Future advances in antimicrobial therapy are exploring novel agents that enhance the efficacy of antifungal and bacteriostatic treatments by targeting specific microbial pathways with minimal resistance development. Innovations in drug delivery systems, such as nanoparticle carriers and controlled-release formulations, improve bioavailability and tissue penetration of antifungal and bacteriostatic compounds. The integration of genomics and artificial intelligence aids in the rapid identification and design of new molecules, optimizing antimicrobial specificity while reducing adverse effects.
Antifungal Infographic
 libterm.com
libterm.com