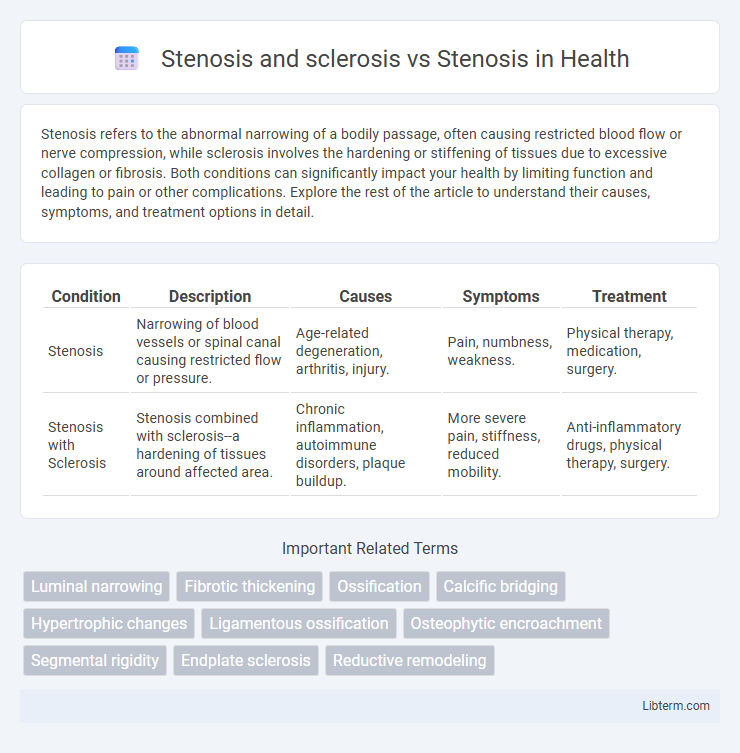
Stenosis refers to the abnormal narrowing of a bodily passage, often causing restricted blood flow or nerve compression, while sclerosis involves the hardening or stiffening of tissues due to excessive collagen or fibrosis. Both conditions can significantly impact your health by limiting function and leading to pain or other complications. Explore the rest of the article to understand their causes, symptoms, and treatment options in detail.
Table of Comparison
| Condition | Description | Causes | Symptoms | Treatment |
|---|---|---|---|---|
| Stenosis | Narrowing of blood vessels or spinal canal causing restricted flow or pressure. | Age-related degeneration, arthritis, injury. | Pain, numbness, weakness. | Physical therapy, medication, surgery. |
| Stenosis with Sclerosis | Stenosis combined with sclerosis--a hardening of tissues around affected area. | Chronic inflammation, autoimmune disorders, plaque buildup. | More severe pain, stiffness, reduced mobility. | Anti-inflammatory drugs, physical therapy, surgery. |
Understanding Stenosis: Definition and Causes
Stenosis refers to the abnormal narrowing of blood vessels or other tubular structures in the body, often leading to restricted blood flow or impaired function. Sclerosis involves the hardening or thickening of tissues, which can contribute to stenosis by causing rigidity and reduced elasticity in affected vessels or ducts. Understanding the causes of stenosis includes recognizing factors such as atherosclerosis, inflammation, congenital defects, and degenerative changes that lead to structural narrowing and increased pressure within the affected area.
Overview of Sclerosis in Medical Contexts
Sclerosis refers to the abnormal hardening of body tissues, often resulting from chronic inflammation, fibrosis, or increased collagen deposition, which can affect organs such as arteries (arteriosclerosis) or the brain (multiple sclerosis). In contrast, stenosis specifically denotes the narrowing or constriction of blood vessels or bodily passages, which can impede normal flow functions. Understanding sclerosis involves recognizing its role in tissue rigidity and loss of elasticity, contributing to disease progression different from the mechanical obstruction seen in stenosis.
Comparing Stenosis and Sclerosis: Key Differences
Stenosis refers to the abnormal narrowing of blood vessels or other tubular structures, often causing restricted blood flow and symptoms like pain or organ dysfunction. Sclerosis involves the hardening or thickening of tissues, primarily due to excessive collagen deposition, which can lead to stiffness and loss of elasticity in affected areas. While stenosis primarily impacts the lumen size causing obstruction, sclerosis affects tissue consistency and structure, often contributing to secondary stenotic changes.
Stenosis Alone: Types and Clinical Implications
Stenosis refers to the abnormal narrowing of blood vessels or tubular organs, commonly seen in spinal stenosis, carotid artery stenosis, and aortic stenosis, each leading to impaired blood flow or nerve compression with significant clinical symptoms. Unlike sclerosis, which involves the hardening or thickening of tissue, stenosis primarily impacts the lumen size, causing ischemia, pain, or neurological deficits depending on the affected area. Understanding the specific type of stenosis is crucial for diagnosis and treatment, as spinal stenosis may require decompression surgery, whereas vascular stenosis often demands angioplasty or stenting to restore proper circulation.
Stenosis and Sclerosis: When Conditions Overlap
Stenosis and sclerosis often coexist, with stenosis referring to the abnormal narrowing of blood vessels or spinal canals, while sclerosis indicates the hardening or stiffening of tissues, frequently due to fibrosis or calcification. This overlap complicates diagnosis and treatment, as sclerosis can exacerbate stenotic conditions by reducing vessel or canal flexibility, thereby intensifying symptoms like pain, numbness, or reduced blood flow. Understanding the interplay between stenosis and sclerosis is crucial for tailored interventions in cardiovascular disease, spinal disorders, and other related pathologies.
Diagnostic Approaches: Stenosis vs Stenosis with Sclerosis
Diagnostic approaches for stenosis primarily involve imaging techniques such as X-rays, MRI, and CT scans to identify the narrowing of blood vessels or spinal canals. When stenosis is accompanied by sclerosis, diagnostic evaluations include bone density assessments and advanced imaging like bone scans or dual-energy X-ray absorptiometry (DEXA) to detect abnormal hardening and thickening of bone tissues. Differentiating between simple stenosis and stenosis with sclerosis is critical for accurate diagnosis and treatment planning, as sclerosis indicates additional pathological bone changes requiring targeted interventions.
Symptoms: Distinguishing Stenosis from Sclerosis-Related Stenosis
Stenosis typically presents with symptoms such as pain, numbness, and muscle weakness due to narrowing of blood vessels or spinal canals, restricting blood flow or nerve function. Sclerosis-related stenosis, often caused by tissue hardening or thickening, may intensify these symptoms by further compressing nerves or vessels, leading to increased stiffness and limited mobility. Recognizing the gradual onset of stiffness and reduced flexibility alongside typical stenosis symptoms can help differentiate sclerosis-related stenosis from simple stenosis.
Treatment Strategies: Stenosis Only vs Stenosis with Sclerosis
Treatment strategies for stenosis alone typically involve physical therapy, anti-inflammatory medications, and, in severe cases, surgical decompression to relieve nerve pressure. In contrast, stenosis with sclerosis requires a more complex approach combining medication to manage bone hardening, such as bisphosphonates or corticosteroids, alongside interventions targeting stenotic narrowing, potentially including osteotomy or spinal fusion. The presence of sclerosis complicates treatment due to altered bone remodeling and reduced vascularity, necessitating tailored rehabilitation and monitoring protocols.
Prognosis and Long-term Outcomes: Is Sclerosis a Risk Factor?
Sclerosis, characterized by abnormal hardening of tissue, is often linked to worse prognosis and long-term outcomes when present alongside stenosis, which refers to the narrowing of blood vessels or valves. Research indicates that sclerosis can exacerbate the pathological progression of stenosis by promoting fibrosis and calcification, increasing the risk of cardiovascular events and reducing vessel elasticity. Patients with stenosis combined with sclerosis typically experience higher rates of morbidity and mortality compared to stenosis alone, positioning sclerosis as a significant risk factor in clinical assessments.
Patient Care Considerations: Managing Complex Cases
In managing complex cases involving both stenosis and sclerosis, patient care requires a comprehensive approach addressing arterial narrowing and vessel wall hardening simultaneously to prevent ischemic complications. Treatment plans often combine pharmacologic therapies like antiplatelet agents and statins with lifestyle modifications and regular imaging to monitor progression. Coordination among cardiologists, neurologists, and vascular specialists is essential to optimize outcomes and tailor interventions based on the severity and location of vascular lesions.
Stenosis and sclerosis Infographic
 libterm.com
libterm.com