Chondromalacia involves the softening and deterioration of cartilage beneath the kneecap, often causing pain during movement, while tendonitis refers to inflammation of a tendon typically resulting from overuse or injury. Both conditions can significantly affect joint function and mobility, requiring targeted treatment strategies to reduce discomfort and promote healing. Explore the full article to understand how to manage and differentiate between chondromalacia and tendonitis effectively.
Table of Comparison
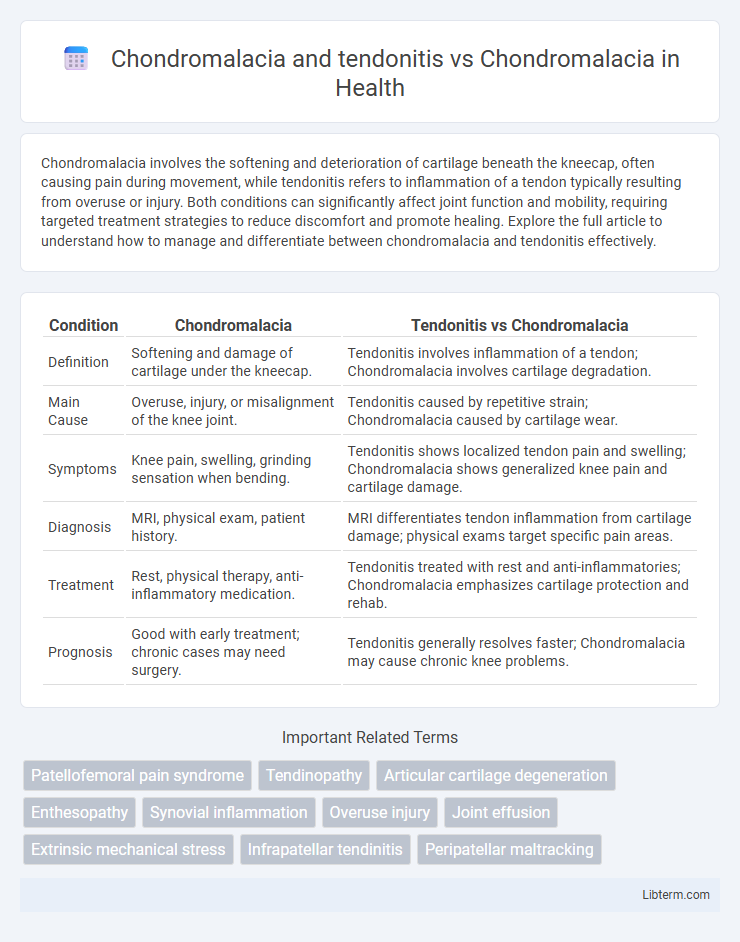
| Condition | Chondromalacia | Tendonitis vs Chondromalacia |
|---|---|---|
| Definition | Softening and damage of cartilage under the kneecap. | Tendonitis involves inflammation of a tendon; Chondromalacia involves cartilage degradation. |
| Main Cause | Overuse, injury, or misalignment of the knee joint. | Tendonitis caused by repetitive strain; Chondromalacia caused by cartilage wear. |
| Symptoms | Knee pain, swelling, grinding sensation when bending. | Tendonitis shows localized tendon pain and swelling; Chondromalacia shows generalized knee pain and cartilage damage. |
| Diagnosis | MRI, physical exam, patient history. | MRI differentiates tendon inflammation from cartilage damage; physical exams target specific pain areas. |
| Treatment | Rest, physical therapy, anti-inflammatory medication. | Tendonitis treated with rest and anti-inflammatories; Chondromalacia emphasizes cartilage protection and rehab. |
| Prognosis | Good with early treatment; chronic cases may need surgery. | Tendonitis generally resolves faster; Chondromalacia may cause chronic knee problems. |
Understanding Chondromalacia: Definition and Causes
Chondromalacia refers to the softening and deterioration of the cartilage on the underside of the kneecap, primarily caused by overuse, injury, or misalignment. Tendonitis involves inflammation of tendons, often resulting from repetitive strain or acute trauma, which can coexist with chondromalacia but affects different tissues. Understanding chondromalacia requires recognizing factors such as cartilage damage due to mechanical stress, improper knee tracking, and weakened muscles contributing to joint pain and mobility issues.
What Is Tendonitis? Key Facts and Symptoms
Tendonitis is the inflammation or irritation of a tendon, often caused by repetitive movements or overuse, leading to pain and tenderness near a joint. Key symptoms include swelling, warmth, and restricted motion around the affected tendon. Unlike chondromalacia, which involves cartilage softening typically in the knee, tendonitis specifically affects tendons and is marked by localized inflammation and discomfort.
Chondromalacia vs Tendonitis: Key Differences
Chondromalacia involves the softening and deterioration of the cartilage under the kneecap, leading to pain and swelling primarily during knee movement. Tendonitis refers to the inflammation or irritation of tendons, causing localized pain and discomfort typically aggravated by repetitive motion or overuse. Key differences include that chondromalacia affects cartilage integrity, whereas tendonitis impacts tendon health, and treatments vary from cartilage repair and physical therapy to anti-inflammatory measures and rest for tendonitis.
Common Risk Factors for Chondromalacia and Tendonitis
Common risk factors for chondromalacia and tendonitis include repetitive knee stress, overuse during physical activities, and biomechanical imbalances such as misalignment or muscle weakness. Both conditions are often associated with age-related cartilage degeneration and previous joint injuries that compromise the structural integrity of the knee. Excessive strain from activities like running, jumping, or cycling further increases the likelihood of developing chondromalacia or tendonitis.
Shared Symptoms and Overlapping Manifestations
Chondromalacia and tendonitis both present with shared symptoms such as joint pain, tenderness, and swelling around the affected area. These conditions often exhibit overlapping manifestations like stiffness and limited range of motion, complicating differential diagnosis. Identifying subtle differences in symptom onset and location is crucial for accurate treatment planning.
Diagnostic Approaches: Chondromalacia vs Tendonitis
Diagnostic approaches for chondromalacia primarily involve MRI scans to detect cartilage softening and degradation within the knee joint, while tendonitis diagnosis relies more on ultrasound imaging and physical examination to identify tendon inflammation and microtears. Both conditions utilize clinical assessment for symptom evaluation, but chondromalacia often requires arthroscopy for definitive diagnosis. Biomarkers and patient history also assist in differentiating cartilage damage in chondromalacia from tendon inflammation in tendonitis.
Treatment Strategies for Chondromalacia
Treatment strategies for chondromalacia primarily involve physical therapy to strengthen the quadriceps and improve knee alignment, reducing cartilage stress. Nonsteroidal anti-inflammatory drugs (NSAIDs) and activity modification help alleviate pain and inflammation associated with chondromalacia. In contrast to tendonitis, which often requires targeted tendon rest and possibly corticosteroid injections, chondromalacia's management focuses more on joint stabilization and cartilage preservation techniques.
Managing Tendonitis: Effective Therapies
Managing tendonitis associated with chondromalacia involves targeted therapies such as physical therapy to strengthen surrounding muscles and reduce joint stress. Anti-inflammatory medications and corticosteroid injections can alleviate pain and inflammation, promoting recovery. Incorporating rest, ice application, and gradual return to activity helps prevent tendon overuse and supports long-term joint health.
Prevention Tips for Chondromalacia and Tendonitis
Preventing chondromalacia and tendonitis involves strengthening the muscles around the knee and maintaining proper joint alignment through targeted exercises like quadriceps and hamstring strengthening. Using proper technique during physical activities and wearing supportive footwear reduces stress on the patella and tendons, minimizing risk. Regular stretching, avoiding overuse, and incorporating rest periods help maintain cartilage health and prevent inflammation of tendons associated with these conditions.
Prognosis and Long-Term Outcomes: Comparative Overview
Chondromalacia often results in softening and damage to the cartilage under the patella, leading to chronic knee pain with a generally favorable prognosis if managed early through physical therapy and activity modification. Tendonitis involves inflammation of tendons, such as the patellar or Achilles tendons, and typically features a quicker recovery timeline but carries a risk of recurring symptoms if the underlying biomechanical issues are not addressed. Long-term outcomes of chondromalacia can include persistent joint discomfort and potential progression to osteoarthritis, whereas tendonitis usually resolves without permanent damage but may necessitate prolonged rehabilitation to prevent recurrence.
Chondromalacia and tendonitis Infographic
 libterm.com
libterm.com