Gastroparesis and gastritis are digestive disorders that affect stomach function and cause symptoms like nausea, abdominal pain, and bloating. Both conditions disrupt normal digestion but have different underlying causes, with gastroparesis involving delayed stomach emptying and gastritis characterized by inflammation of the stomach lining. To understand how these ailments impact your health and explore effective treatment options, continue reading the rest of the article.
Table of Comparison
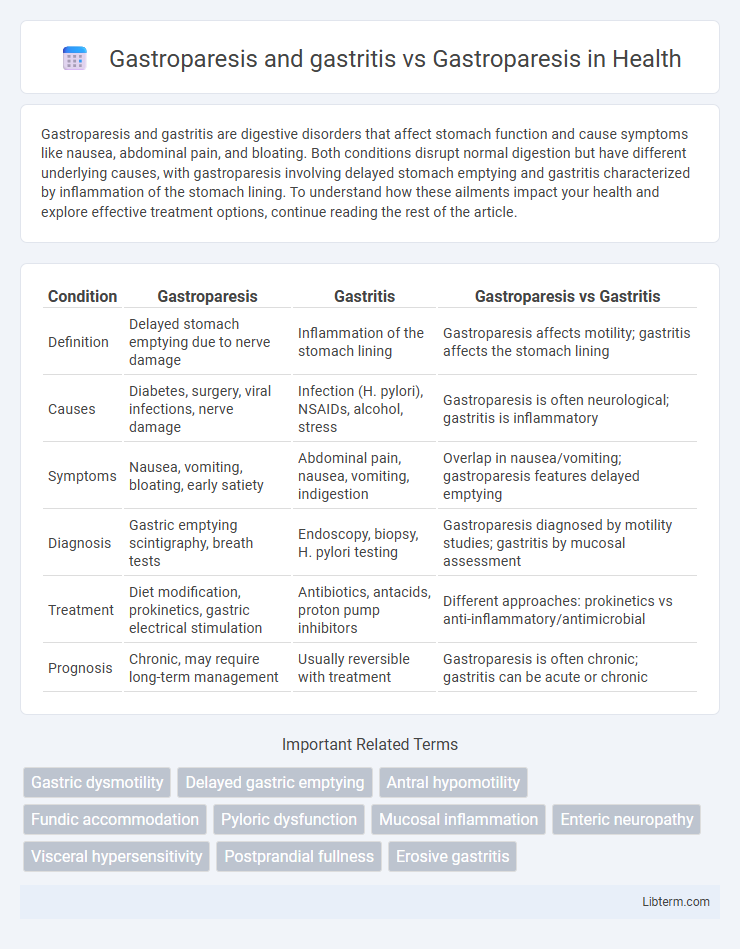
| Condition | Gastroparesis | Gastritis | Gastroparesis vs Gastritis |
|---|---|---|---|
| Definition | Delayed stomach emptying due to nerve damage | Inflammation of the stomach lining | Gastroparesis affects motility; gastritis affects the stomach lining |
| Causes | Diabetes, surgery, viral infections, nerve damage | Infection (H. pylori), NSAIDs, alcohol, stress | Gastroparesis is often neurological; gastritis is inflammatory |
| Symptoms | Nausea, vomiting, bloating, early satiety | Abdominal pain, nausea, vomiting, indigestion | Overlap in nausea/vomiting; gastroparesis features delayed emptying |
| Diagnosis | Gastric emptying scintigraphy, breath tests | Endoscopy, biopsy, H. pylori testing | Gastroparesis diagnosed by motility studies; gastritis by mucosal assessment |
| Treatment | Diet modification, prokinetics, gastric electrical stimulation | Antibiotics, antacids, proton pump inhibitors | Different approaches: prokinetics vs anti-inflammatory/antimicrobial |
| Prognosis | Chronic, may require long-term management | Usually reversible with treatment | Gastroparesis is often chronic; gastritis can be acute or chronic |
Understanding Gastroparesis: Definition and Causes
Gastroparesis is a chronic digestive disorder characterized by delayed stomach emptying without any mechanical obstruction, often caused by nerve damage, diabetes, or infections. Gastritis involves inflammation of the stomach lining, usually due to infections like Helicobacter pylori or prolonged NSAID use, which differs from the neuromuscular dysfunction seen in gastroparesis. Understanding these distinctions highlights gastroparesis as a motility disorder primarily linked to autonomic neuropathy, while gastritis centers on mucosal inflammation and irritation.
What is Gastritis? Symptoms and Triggers
Gastritis is the inflammation of the stomach lining, often caused by infections such as Helicobacter pylori, prolonged use of NSAIDs, or excessive alcohol consumption. Common symptoms include abdominal pain, nausea, vomiting, and indigestion, while triggers may involve spicy foods, stress, and certain medications. Unlike gastroparesis, which involves delayed stomach emptying, gastritis primarily affects the stomach's mucosal layer, leading to irritation and discomfort without necessarily impairing gastric motility.
Gastroparesis Alone: Clinical Presentation
Gastroparesis, characterized by delayed gastric emptying without mechanical obstruction, presents clinically with symptoms such as nausea, vomiting, early satiety, and abdominal pain. Unlike gastritis, which involves mucosal inflammation, gastroparesis primarily disrupts gastric motility and autonomic function, leading to nutritional deficiencies and weight loss. Diagnostic evaluation often includes gastric emptying studies, emphasizing the importance of differentiating motility disorders from inflammatory gastric conditions for targeted management.
Comparing Gastroparesis and Gastritis: Key Differences
Gastroparesis and gastritis both affect the stomach but differ significantly in cause and symptoms; gastroparesis involves delayed gastric emptying due to nerve damage, often linked to diabetes, while gastritis is inflammation of the stomach lining primarily caused by infections, NSAIDs, or alcohol. Gastroparesis symptoms include nausea, vomiting, and bloating related to impaired stomach motility, whereas gastritis commonly presents with abdominal pain, indigestion, and possible bleeding. Diagnosis relies on gastric emptying studies for gastroparesis and endoscopy or biopsy for gastritis, guiding distinct treatment approaches focusing on motility enhancement versus inflammation reduction.
Shared and Unique Symptoms: Gastroparesis vs. Gastritis
Gastroparesis and gastritis both involve stomach dysfunction but differ in pathophysiology and symptom presentation. Common symptoms include nausea, abdominal pain, and bloating, while gastroparesis uniquely causes delayed gastric emptying leading to early satiety and vomiting, and gastritis specifically presents with mucosal inflammation resulting in upper abdominal discomfort and possible gastrointestinal bleeding. Accurate differentiation through diagnostic tests like gastric emptying studies for gastroparesis and endoscopy for gastritis enhances targeted treatment strategies.
Overlapping Conditions: When Gastroparesis and Gastritis Coexist
Gastroparesis and gastritis frequently coexist, complicating diagnosis and treatment due to overlapping symptoms such as nausea, abdominal pain, and bloating. Both conditions involve delayed gastric emptying and inflammation, which can exacerbate gastrointestinal distress and impair nutrient absorption. Managing patients with concurrent gastroparesis and gastritis requires targeted therapies addressing motility disorders and mucosal inflammation to improve clinical outcomes.
Diagnostic Challenges: Differentiating Gastroparesis from Gastritis
Gastroparesis and gastritis share overlapping symptoms such as nausea, vomiting, and abdominal pain, complicating accurate diagnosis. Gastroparesis is characterized by delayed gastric emptying without mechanical obstruction, which requires specialized tests like gastric emptying scintigraphy, while gastritis involves inflammation of the stomach lining confirmed by endoscopic biopsy. Differentiating these conditions is crucial as their pathophysiology, treatment approaches, and prognoses differ significantly, necessitating precise diagnostic strategies.
Complications Arising from Combined Gastroparesis and Gastritis
Complications arising from combined gastroparesis and gastritis often include severe gastric stasis and increased risk of gastric ulcers due to prolonged acid exposure and impaired gastric motility. This combination exacerbates symptoms such as nausea, vomiting, and abdominal pain, and raises the likelihood of malnutrition and electrolyte imbalances. Chronic inflammation from gastritis further impairs gastric emptying, complicating management and increasing the risk of gastroparesis-related complications like bezoar formation and severe gastroparesis symptoms.
Treatment Approaches: Managing Gastroparesis vs. Managing Both Conditions
Treatment approaches for managing gastroparesis primarily focus on dietary modifications, prokinetic medications like metoclopramide, and in severe cases, gastric electrical stimulation or feeding tubes. Managing both gastroparesis and gastritis requires a combined strategy including acid-suppressing agents such as proton pump inhibitors or H2 blockers to reduce inflammation, alongside prokinetics to improve gastric motility. Effective management involves addressing delayed gastric emptying and mucosal inflammation simultaneously to alleviate symptoms and enhance digestive function.
Lifestyle Modifications for Gastroparesis and Gastritis Patients
Gastroparesis and gastritis both benefit from lifestyle modifications that aim to reduce symptoms and improve digestive health. Small, frequent meals low in fat and fiber help minimize gastric emptying delays in gastroparesis while soothing inflamed stomach lining in gastritis. Avoiding alcohol, smoking, and NSAIDs supports mucosal healing in gastritis and prevents symptom exacerbation in gastroparesis patients.
Gastroparesis and gastritis Infographic
 libterm.com
libterm.com