Fibrosis is the excessive formation of connective tissue, leading to the hardening and scarring of organs such as the liver, lungs, or heart. This abnormal tissue growth disrupts normal organ function and can result in chronic health issues if left untreated. Discover how fibrosis impacts your body and explore effective strategies for management by reading the rest of this article.
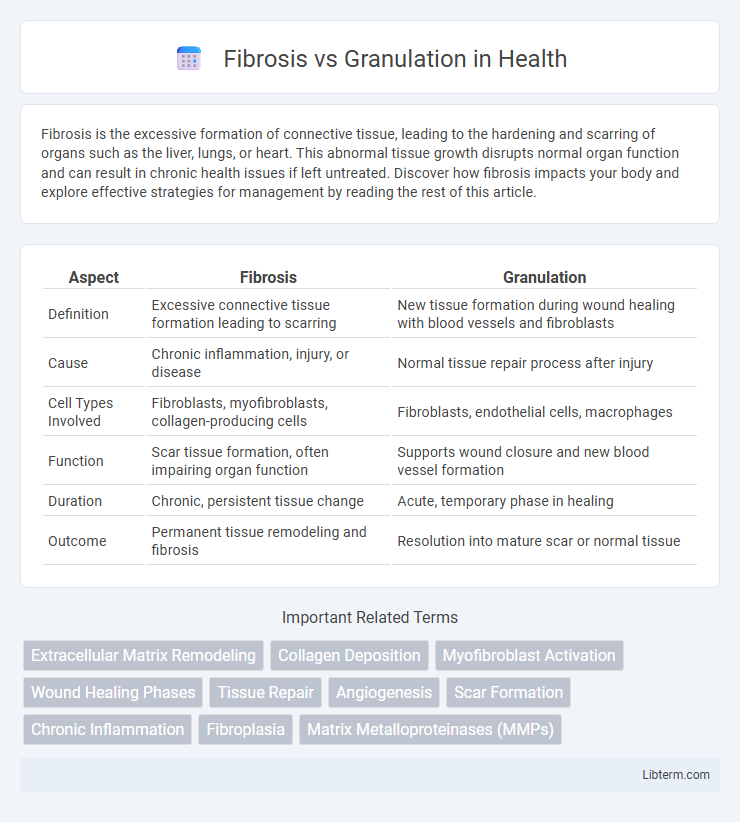
Table of Comparison
| Aspect | Fibrosis | Granulation |
|---|---|---|
| Definition | Excessive connective tissue formation leading to scarring | New tissue formation during wound healing with blood vessels and fibroblasts |
| Cause | Chronic inflammation, injury, or disease | Normal tissue repair process after injury |
| Cell Types Involved | Fibroblasts, myofibroblasts, collagen-producing cells | Fibroblasts, endothelial cells, macrophages |
| Function | Scar tissue formation, often impairing organ function | Supports wound closure and new blood vessel formation |
| Duration | Chronic, persistent tissue change | Acute, temporary phase in healing |
| Outcome | Permanent tissue remodeling and fibrosis | Resolution into mature scar or normal tissue |
Understanding Fibrosis: Definition and Mechanisms
Fibrosis is the excessive accumulation of extracellular matrix proteins, primarily collagen, leading to tissue scarring and impaired organ function. It results from chronic inflammation or injury where activated fibroblasts proliferate and deposit collagen, disrupting normal tissue architecture. Understanding fibrosis involves studying cellular signaling pathways such as TGF-b that regulate fibroblast activation and extracellular matrix production.
What is Granulation Tissue? Key Characteristics
Granulation tissue is a vital component of the healing process, characterized by the proliferation of new connective tissue and tiny blood vessels that form on the surfaces of a wound. It consists primarily of fibroblasts, endothelial cells, and inflammatory cells, facilitating angiogenesis and extracellular matrix deposition. Unlike fibrosis, granulation tissue is a temporary, dynamic structure that gradually matures and remodels into scar tissue during wound repair.
Cellular Composition: Fibrosis vs Granulation
Fibrosis is characterized by the excessive accumulation of fibroblasts and myofibroblasts, along with dense collagen deposition leading to scar tissue formation. Granulation tissue consists primarily of proliferating fibroblasts, numerous new capillaries formed by endothelial cells, and a rich presence of inflammatory cells such as macrophages and neutrophils. Unlike fibrosis, granulation tissue represents an active reparative phase with abundant extracellular matrix remodeling and neovascularization.
Causes and Triggers: How Each Process Begins
Fibrosis begins as a response to chronic inflammation or persistent tissue injury, where activated fibroblasts produce excessive extracellular matrix components like collagen, leading to scar formation and tissue stiffening. Granulation forms during the early phases of wound healing, triggered by acute injury and characterized by the proliferation of new capillaries, fibroblasts, and immune cells to restore tissue integrity. The key difference lies in fibrosis being driven by unresolved or repeated damage causing pathological scarring, while granulation is a controlled, reparative process initiating immediate tissue repair.
Physiological Role in Healing and Disease
Fibrosis involves excessive deposition of extracellular matrix proteins, leading to tissue scarring and impaired organ function, commonly seen in chronic diseases like liver cirrhosis and pulmonary fibrosis. Granulation tissue forms as a temporary matrix during wound healing, characterized by proliferating fibroblasts, new capillaries, and inflammatory cells crucial for tissue repair and regeneration. The physiological role of granulation is to restore tissue integrity, whereas fibrosis represents a pathological process where unresolved inflammation results in permanent tissue remodeling and dysfunction.
Visual and Histological Differences
Fibrosis appears visually as dense, white scar tissue, whereas granulation tissue is typically red or pink due to its rich vascularity. Histologically, fibrosis is characterized by the accumulation of dense collagen fibers and fewer cells, indicating tissue repair and scarring, while granulation tissue displays abundant fibroblasts, new capillaries, and inflammatory cells, reflecting active tissue regeneration. The presence of myofibroblasts in fibrosis contributes to wound contraction, unlike granulation tissue, which is more cellular and less rigid in structure.
Clinical Implications of Fibrosis
Fibrosis is characterized by excessive deposition of extracellular matrix proteins leading to tissue scarring and impaired organ function, whereas granulation tissue represents a temporary, highly vascularized phase of wound healing. Clinically, fibrosis is associated with chronic diseases such as pulmonary fibrosis, liver cirrhosis, and cardiac fibrosis, resulting in irreversible tissue remodeling and decreased physiological function. Early detection and intervention targeting fibrotic pathways are critical to prevent progression and preserve organ integrity.
Importance of Granulation in Wound Healing
Granulation tissue formation is a critical phase in wound healing, characterized by the proliferation of new blood vessels, fibroblasts, and extracellular matrix, which provides a foundation for tissue repair. Unlike fibrosis, which results in excessive scar tissue and impaired function, granulation promotes organized tissue regeneration and restores skin integrity. Effective granulation ensures sufficient oxygenation and nutrient delivery to the wound bed, accelerating healing and reducing the risk of chronic wounds.
Diagnostic Techniques: Differentiating Fibrosis from Granulation
Differentiating fibrosis from granulation tissue relies heavily on histopathological analysis using specialized staining techniques such as Masson's trichrome and reticulin stains, which highlight collagen deposition indicative of fibrosis. Imaging modalities including ultrasound elastography and MRI provide non-invasive assessment by detecting tissue stiffness and structural characteristics, with fibrosis presenting as denser, less vascularized tissue compared to the highly vascular granulation tissue. Immunohistochemical markers like a-smooth muscle actin (a-SMA) and CD34 further aid in distinguishing myofibroblast-rich fibrotic areas from endothelial cell-rich granulation tissue during diagnostic evaluation.
Treatment Approaches and Prognosis
Fibrosis treatment primarily involves antifibrotic agents, corticosteroids, and addressing underlying causes to limit scar tissue formation, while granulation tissue management focuses on promoting healthy wound healing through debridement, moisture control, and sometimes topical growth factors. Prognosis of fibrosis varies with the extent of organ involvement and response to therapy, often leading to permanent tissue stiffening, whereas granulation tissue typically resolves with effective wound care, resulting in tissue regeneration. Early intervention is critical in both conditions to improve outcomes and minimize complications.
Fibrosis Infographic
 libterm.com
libterm.com