Gastroesophageal reflux occurs when stomach acid flows back into the esophagus, causing discomfort and potential damage to the esophageal lining. Common symptoms include heartburn, regurgitation, and difficulty swallowing, which can impact your daily life if left untreated. Discover effective treatments and lifestyle adjustments to manage gastroesophageal reflux by reading the full article.
Table of Comparison
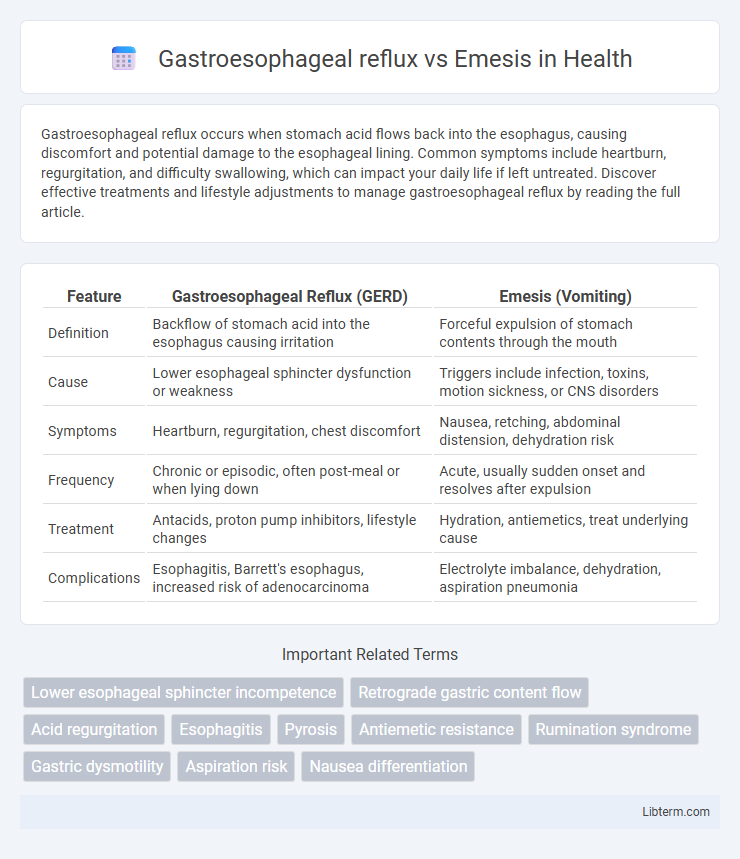
| Feature | Gastroesophageal Reflux (GERD) | Emesis (Vomiting) |
|---|---|---|
| Definition | Backflow of stomach acid into the esophagus causing irritation | Forceful expulsion of stomach contents through the mouth |
| Cause | Lower esophageal sphincter dysfunction or weakness | Triggers include infection, toxins, motion sickness, or CNS disorders |
| Symptoms | Heartburn, regurgitation, chest discomfort | Nausea, retching, abdominal distension, dehydration risk |
| Frequency | Chronic or episodic, often post-meal or when lying down | Acute, usually sudden onset and resolves after expulsion |
| Treatment | Antacids, proton pump inhibitors, lifestyle changes | Hydration, antiemetics, treat underlying cause |
| Complications | Esophagitis, Barrett's esophagus, increased risk of adenocarcinoma | Electrolyte imbalance, dehydration, aspiration pneumonia |
Introduction to Gastroesophageal Reflux and Emesis
Gastroesophageal reflux (GER) is the backward flow of stomach contents into the esophagus, often causing heartburn and discomfort due to the irritation of the esophageal lining. Emesis, commonly known as vomiting, is the forceful expulsion of stomach contents through the mouth, triggered by various stimuli such as gastrointestinal infections, motion sickness, or central nervous system disorders. Differentiating GER from emesis is crucial, as GER primarily involves acid reflux without forceful expulsion, while emesis presents with active vomiting episodes.
Defining Gastroesophageal Reflux
Gastroesophageal reflux (GER) occurs when stomach acid flows back into the esophagus, causing symptoms like heartburn and regurgitation due to weakened lower esophageal sphincter function. Emesis, commonly known as vomiting, involves the forceful expulsion of stomach contents through the mouth and is a distinct physiological process from GER. Understanding GER is crucial for diagnosing conditions like gastroesophageal reflux disease (GERD), which can lead to esophageal inflammation and complications if untreated.
Understanding Emesis: Causes and Mechanisms
Emesis, or vomiting, is the forceful expulsion of stomach contents through the mouth triggered by signals in the brain's vomiting center, often due to stimuli such as infections, gastrointestinal irritation, or central nervous system disorders. Unlike gastroesophageal reflux, which involves the backflow of stomach acid into the esophagus causing heartburn, emesis involves coordinated muscular contractions in the diaphragm, abdominal wall, and gastrointestinal tract. Recognizing the distinct mechanisms and causes, including chemical triggers like toxins or vestibular disturbances, helps differentiate emesis from the acid reflux process.
Key Differences Between Reflux and Emesis
Gastroesophageal reflux involves the backward flow of stomach acid into the esophagus, causing symptoms like heartburn and regurgitation, whereas emesis refers to the forceful expulsion of stomach contents through vomiting. Reflux is a chronic condition often linked to gastroesophageal reflux disease (GERD), whereas emesis is typically an acute response triggered by factors such as infections, toxins, or motion sickness. Key differences include the mechanism, with reflux being a passive backflow and emesis an active reflex, and the clinical presentation--reflux rarely leads to visible vomitus, while emesis results in the observable ejection of stomach contents.
Common Symptoms of Reflux vs. Emesis
Gastroesophageal reflux commonly presents with symptoms such as heartburn, regurgitation, and chest discomfort due to the backflow of stomach acid into the esophagus. Emesis, or vomiting, is characterized by the forceful expulsion of stomach contents through the mouth, often accompanied by nausea and abdominal pain. While reflux symptoms are chronic and related to acid irritation, emesis is typically an acute event signaling gastrointestinal distress or obstruction.
Triggers and Risk Factors
Gastroesophageal reflux is primarily triggered by factors such as dietary choices including fatty and spicy foods, obesity, hiatal hernia, and delayed gastric emptying, increasing acid exposure in the esophagus. Emesis, or vomiting, is often caused by a broader range of triggers including infections, gastrointestinal obstructions, central nervous system disorders, motion sickness, and certain medications. Risk factors for gastroesophageal reflux include age, pregnancy, and smoking, while emesis risk factors are more variable and depend on the underlying cause such as infections, toxins, or neurological conditions.
Diagnostic Approaches for Each Condition
Gastroesophageal reflux is diagnosed primarily through esophageal pH monitoring, upper endoscopy, and esophageal manometry to assess acid exposure and esophageal motility. Emesis diagnosis involves identifying underlying causes using clinical history, physical examination, and laboratory tests such as electrolyte panels, imaging studies like abdominal ultrasound or CT scans, and, in some cases, upper gastrointestinal endoscopy. Both conditions require tailored diagnostic approaches based on symptom severity and associated clinical findings to guide effective treatment strategies.
Treatment Options for Gastroesophageal Reflux
Treatment options for gastroesophageal reflux primarily include lifestyle modifications such as dietary changes, weight management, and avoiding trigger foods. Pharmacological interventions involve the use of antacids, H2 receptor blockers, and proton pump inhibitors to reduce stomach acid and promote healing. In severe cases, surgical procedures like fundoplication may be considered to strengthen the lower esophageal sphincter and prevent acid reflux.
Management and Prevention of Emesis
Management of emesis involves the use of antiemetic medications such as ondansetron and metoclopramide to control nausea and vomiting, along with hydration therapy to prevent dehydration. Preventive measures include identifying and avoiding emetic triggers, implementing dietary modifications like small, frequent meals, and addressing underlying causes such as gastrointestinal infections or motion sickness. Behavioral strategies, like maintaining upright posture post-meals, and supportive care in acute settings also play a critical role in reducing the incidence and severity of emesis.
When to Seek Medical Attention
Seek medical attention for gastroesophageal reflux if symptoms persist beyond two weeks, worsen despite lifestyle changes, or include severe chest pain, difficulty swallowing, or unexplained weight loss. Emesis requires prompt medical evaluation if vomiting is frequent, contains blood or bile, or is accompanied by signs of dehydration such as dizziness and reduced urine output. Both conditions demand urgent care when associated with high fever, severe abdominal pain, or altered consciousness to prevent complications.
Gastroesophageal reflux Infographic
 libterm.com
libterm.com