Thrombocytosis is a condition characterized by an elevated platelet count in the blood, which can increase the risk of clotting or bleeding complications. It may result from various causes, including reactive processes or bone marrow disorders, and requires accurate diagnosis for appropriate management. Discover more about the symptoms, causes, and treatment options for thrombocytosis in the rest of this article.
Table of Comparison
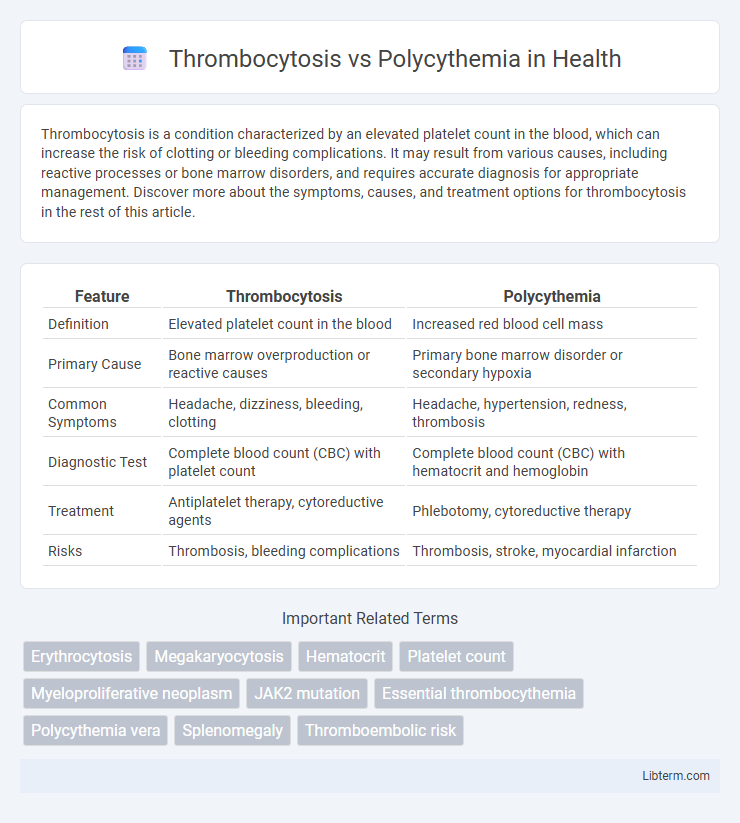
| Feature | Thrombocytosis | Polycythemia |
|---|---|---|
| Definition | Elevated platelet count in the blood | Increased red blood cell mass |
| Primary Cause | Bone marrow overproduction or reactive causes | Primary bone marrow disorder or secondary hypoxia |
| Common Symptoms | Headache, dizziness, bleeding, clotting | Headache, hypertension, redness, thrombosis |
| Diagnostic Test | Complete blood count (CBC) with platelet count | Complete blood count (CBC) with hematocrit and hemoglobin |
| Treatment | Antiplatelet therapy, cytoreductive agents | Phlebotomy, cytoreductive therapy |
| Risks | Thrombosis, bleeding complications | Thrombosis, stroke, myocardial infarction |
Understanding Thrombocytosis and Polycythemia
Thrombocytosis is characterized by an elevated platelet count, often exceeding 450,000 platelets per microliter of blood, leading to increased risk of clot formation and bleeding complications. Polycythemia involves an abnormal increase in red blood cell mass, raising hematocrit levels above 52% in men and 48% in women, which thickens the blood and risks thrombosis. Differentiating these conditions requires blood tests including complete blood count (CBC) and bone marrow biopsy to identify underlying causes such as myeloproliferative disorders.
Key Differences: Platelets vs Red Blood Cells
Thrombocytosis is characterized by an excessive increase in platelets, which are crucial for blood clotting, whereas polycythemia involves an elevated red blood cell count, enhancing oxygen transport capacity. Platelet counts in thrombocytosis typically exceed 450,000 per microliter, while polycythemia shows increased hematocrit levels above 52% in men and 48% in women due to red blood cell overproduction. These distinct cellular elevations impact blood viscosity differently, affecting clotting risk in thrombocytosis and oxygen delivery efficiency in polycythemia.
Causes of Thrombocytosis
Thrombocytosis is primarily caused by reactive conditions such as inflammation, infection, or iron deficiency, while polycythemia results from increased red blood cell production often due to polycythemia vera or chronic hypoxia. Essential thrombocythemia, a myeloproliferative neoplasm, is a key cause of persistent thrombocytosis alongside secondary causes linked to diseases like cancer or post-surgery states. Understanding the distinct etiologies aids in differential diagnosis between elevated platelet counts in thrombocytosis and increased red cell mass in polycythemia.
Causes of Polycythemia
Polycythemia primarily results from increased erythropoietin production due to chronic hypoxia, such as in chronic obstructive pulmonary disease (COPD) or living at high altitudes. Secondary causes include erythropoietin-secreting tumors like renal cell carcinoma and hepatocellular carcinoma. Unlike thrombocytosis, which involves elevated platelet count, polycythemia is characterized by an abnormal increase in red blood cells.
Clinical Symptoms and Presentations
Thrombocytosis typically presents with symptoms such as headaches, dizziness, and visual disturbances due to increased platelet count causing microvascular thrombosis. Polycythemia often manifests with symptoms including erythromelalgia, pruritus after a hot shower, and symptoms related to hyperviscosity like blurred vision and hypertension. Both conditions carry risks of thrombotic events, but polycythemia tends to present more prominently with hyperviscosity symptoms, whereas thrombocytosis is more associated with platelet aggregation complications.
Diagnostic Criteria and Laboratory Tests
Thrombocytosis is characterized by a platelet count exceeding 450,000/uL, whereas polycythemia involves an elevated red blood cell mass with a hematocrit greater than 52% in men or 48% in women. Diagnostic criteria for thrombocytosis include ruling out reactive causes and confirming essential thrombocythemia through bone marrow biopsy and JAK2 mutation testing. Polycythemia diagnosis relies on measuring erythropoietin levels, JAK2 V617F mutation analysis, and arterial oxygen saturation to differentiate between primary polycythemia vera and secondary causes.
Complications and Associated Risks
Thrombocytosis increases the risk of thrombosis, leading to complications such as stroke, myocardial infarction, and deep vein thrombosis due to excessive platelet aggregation. Polycythemia elevates blood viscosity and volume, raising the likelihood of vascular occlusion, hypertension, and hemorrhagic events, along with potential progression to myelofibrosis or acute leukemia. Both disorders require careful management to mitigate risks of thrombotic and hemorrhagic complications.
Treatment Approaches and Management
Thrombocytosis treatment primarily targets reducing platelet count through medications such as hydroxyurea or anagrelide, alongside low-dose aspirin to prevent clotting complications. Polycythemia management often involves therapeutic phlebotomy to lower red blood cell mass and drugs like hydroxyurea or interferon-alpha to control bone marrow production. Both conditions require regular monitoring to adjust treatment and minimize risks of thrombosis or hemorrhage.
Prognosis and Long-Term Outcomes
Thrombocytosis, characterized by an elevated platelet count, generally presents a variable prognosis depending on its primary or secondary nature, with essential thrombocythemia carrying a risk of thrombotic events and progression to myelofibrosis or acute leukemia. Polycythemia, especially polycythemia vera, involves increased red blood cell mass and is associated with heightened risks of thrombosis, hemorrhage, and transformation to myelofibrosis or acute myeloid leukemia, impacting long-term survival. Both conditions require careful monitoring and management to mitigate complications and improve long-term outcomes.
When to Seek Medical Attention
Seek medical attention for thrombocytosis if platelet counts exceed 450,000 per microliter, especially when accompanied by symptoms like unexplained bruising, bleeding, or blood clots, which indicate risk of thrombosis. In polycythemia, immediate evaluation is necessary when hematocrit levels rise above 52% in men or 48% in women, or if symptoms such as headache, dizziness, or vision disturbances occur, signaling increased blood viscosity and potential complications. Early diagnosis and treatment are crucial to prevent serious events such as stroke, myocardial infarction, or deep vein thrombosis in both conditions.
Thrombocytosis Infographic
 libterm.com
libterm.com