Dyssomnia refers to a group of sleep disorders characterized by difficulties in falling asleep, staying asleep, or excessive sleepiness during the day, significantly impacting overall health and daily functioning. Common types include insomnia, narcolepsy, and sleep apnea, each requiring specific diagnosis and treatment strategies for effective management. Explore this article to understand dyssomnia symptoms, causes, and the best approaches to improve your sleep quality.
Table of Comparison
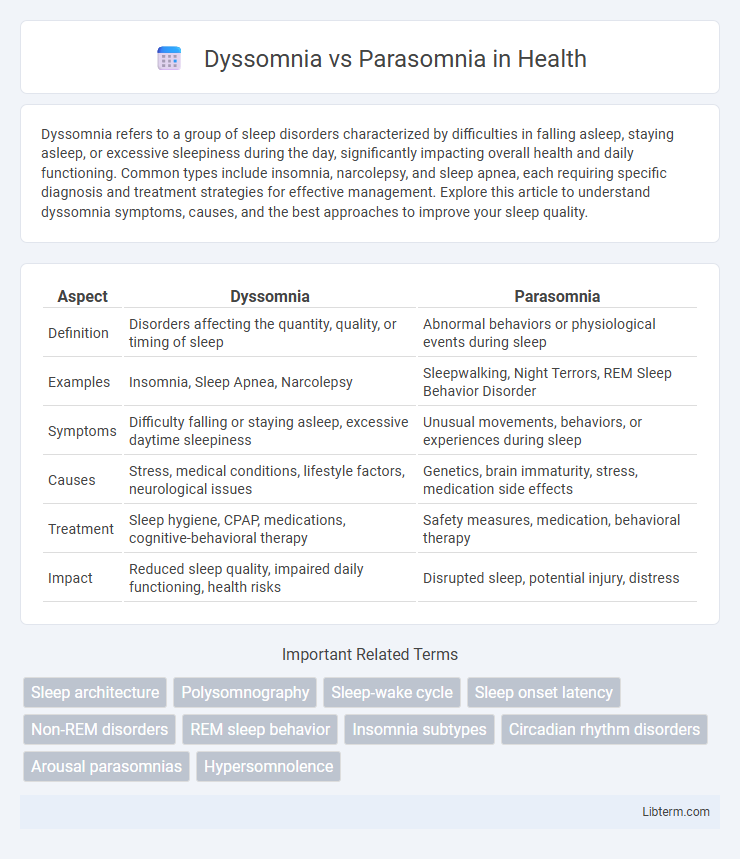
| Aspect | Dyssomnia | Parasomnia |
|---|---|---|
| Definition | Disorders affecting the quantity, quality, or timing of sleep | Abnormal behaviors or physiological events during sleep |
| Examples | Insomnia, Sleep Apnea, Narcolepsy | Sleepwalking, Night Terrors, REM Sleep Behavior Disorder |
| Symptoms | Difficulty falling or staying asleep, excessive daytime sleepiness | Unusual movements, behaviors, or experiences during sleep |
| Causes | Stress, medical conditions, lifestyle factors, neurological issues | Genetics, brain immaturity, stress, medication side effects |
| Treatment | Sleep hygiene, CPAP, medications, cognitive-behavioral therapy | Safety measures, medication, behavioral therapy |
| Impact | Reduced sleep quality, impaired daily functioning, health risks | Disrupted sleep, potential injury, distress |
Introduction to Dyssomnia and Parasomnia
Dyssomnia refers to sleep disorders characterized by difficulties in initiating, maintaining, or obtaining restful sleep, including insomnia, hypersomnia, and sleep apnea. Parasomnia encompasses abnormal behaviors or physiological events occurring during sleep, such as sleepwalking, night terrors, and REM sleep behavior disorder. Both dyssomnia and parasomnia impact sleep quality and overall health but differ in symptoms and underlying mechanisms.
Defining Dyssomnia: Key Characteristics
Dyssomnia encompasses sleep disorders characterized by difficulties in initiating, maintaining, or timing sleep, resulting in excessive daytime sleepiness or impaired sleep quality. Key characteristics include insomnia, hypersomnia, and circadian rhythm sleep disorders, each involving disruptions to the quantity or timing of sleep. Unlike parasomnias, which involve abnormal behaviors during sleep, dyssomnia primarily affects the duration and continuity of sleep cycles.
Understanding Parasomnia: Main Features
Parasomnia involves abnormal behaviors or experiences during sleep, such as sleepwalking, night terrors, and REM sleep behavior disorder, which occur during transitions between sleep stages. These disturbances differ from dyssomnia, which primarily affects the quantity, quality, or timing of sleep, including insomnia and sleep apnea. Understanding parasomnia requires recognizing its episodic, often involuntary nature and its association with disruptive or complex motor activities during sleep disruption.
Types of Dyssomnia Disorders
Dyssomnia disorders primarily include insomnia, characterized by difficulty initiating or maintaining sleep; hypersomnia, marked by excessive daytime sleepiness despite adequate nighttime sleep; and circadian rhythm sleep-wake disorders, involving misalignment between the sleep pattern and the external environment. Other types include narcolepsy, which causes sudden sleep attacks, and sleep apnea, where breathing repeatedly stops and starts during sleep. Understanding these specific dyssomnia types aids in accurate diagnosis and targeted treatment for disrupted sleep patterns.
Common Forms of Parasomnia
Parasomnias encompass a range of disruptive sleep disorders, including sleepwalking, night terrors, and REM sleep behavior disorder, characterized by abnormal movements, behaviors, emotions, or perceptions during sleep transitions. Unlike dyssomnias, which primarily involve difficulties in initiating or maintaining sleep, parasomnias manifest through unusual physical or verbal activities. Understanding parasomnia types aids in targeted treatment and accurate differentiation from dyssomnia-related sleep disturbances.
Causes and Risk Factors: Dyssomnia vs Parasomnia
Dyssomnia primarily results from disruptions in the circadian rhythm, stress, or medical conditions such as insomnia and sleep apnea, with risk factors including age, mental health disorders, and lifestyle habits like irregular sleep schedules. Parasomnia arises from abnormal behaviors during sleep, often caused by genetic predisposition, neurological conditions, or environmental stressors, and risk factors include sleep deprivation, high arousal threshold, and specific medications. Understanding these distinct causes and risk profiles aids in targeted diagnosis and treatment for dyssomnia and parasomnia.
Symptoms: Comparative Overview
Dyssomnia primarily manifests through symptoms such as difficulty falling asleep, frequent awakenings, and excessive daytime sleepiness, indicating disruptions in the amount or quality of sleep. Parasomnia involves abnormal behaviors during sleep, including sleepwalking, night terrors, and REM sleep behavior disorder, characterized by unusual physical activities or experiences. Both conditions affect sleep architecture but differ substantially in symptom presentation and underlying mechanisms.
Diagnosis and Assessment Methods
Dyssomnia is diagnosed through detailed sleep history evaluations and polysomnography to identify difficulties in sleep initiation or maintenance, such as insomnia or hypersomnia, whereas parasomnia diagnosis relies heavily on video EEG monitoring and patient-reported behaviors during sleep, like sleepwalking or night terrors. Actigraphy and sleep diaries complement the assessment of dyssomnias by tracking sleep patterns over extended periods. Parasomnia assessments may also employ multiple sleep latency tests (MSLT) to distinguish between various REM-related phenomena and neurological conditions.
Treatment Approaches for Each Condition
Dyssomnia treatment primarily involves cognitive-behavioral therapy (CBT), medication such as melatonin or sedatives, and improving sleep hygiene to regulate sleep-wake cycles. Parasomnia management focuses on ensuring safety during episodes, behavioral strategies like scheduled awakenings for night terrors, and medications including benzodiazepines or antidepressants depending on the specific parasomnia subtype. Both conditions may require multidisciplinary approaches including neurologists or sleep specialists to tailor individualized treatment plans.
Preventive Strategies and Sleep Hygiene Tips
Dyssomnia prevention centers on maintaining consistent sleep schedules, limiting caffeine and electronic device use before bedtime, and creating a dark, quiet, and comfortable sleep environment to enhance sleep quality. Parasomnia management emphasizes safety measures such as securing the sleep area, using protective bedding, and avoiding substances that may trigger episodes like alcohol or certain medications. Adopting comprehensive sleep hygiene practices, including regular physical activity and stress reduction techniques, supports overall restorative sleep and reduces the risk of both dyssomnias and parasomnias.
Dyssomnia Infographic
 libterm.com
libterm.com