Beta-cell function plays a crucial role in maintaining blood glucose levels by producing and secreting insulin in response to rising glucose concentrations. Impaired beta-cell function can lead to inadequate insulin release, contributing to the development of type 2 diabetes and other metabolic disorders. Explore the rest of the article to understand how optimizing beta-cell function can improve your overall metabolic health.
Table of Comparison
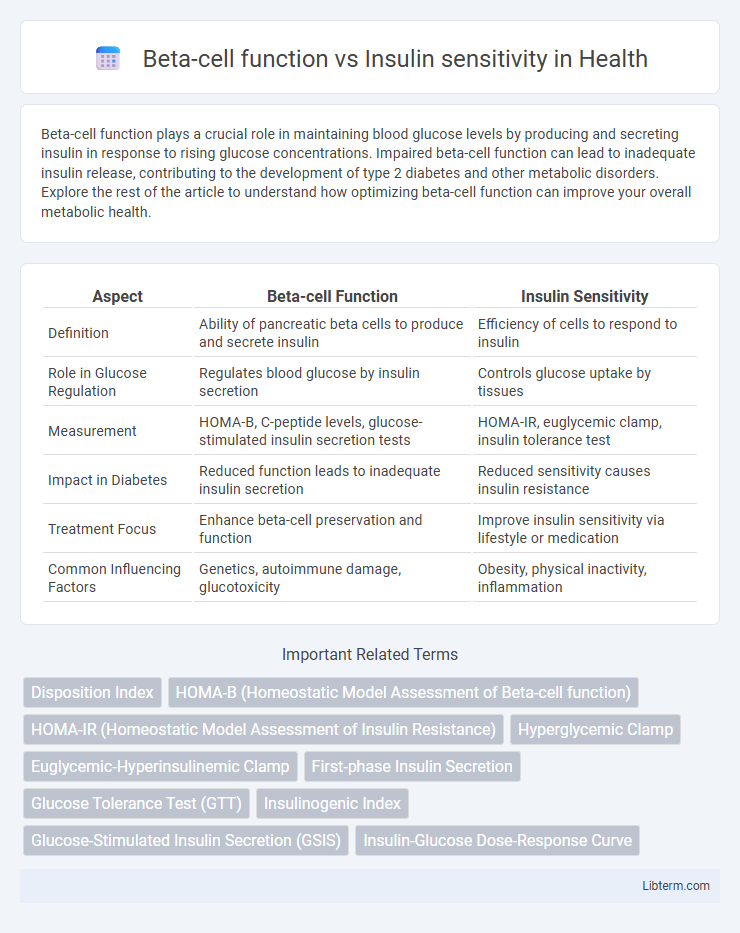
| Aspect | Beta-cell Function | Insulin Sensitivity |
|---|---|---|
| Definition | Ability of pancreatic beta cells to produce and secrete insulin | Efficiency of cells to respond to insulin |
| Role in Glucose Regulation | Regulates blood glucose by insulin secretion | Controls glucose uptake by tissues |
| Measurement | HOMA-B, C-peptide levels, glucose-stimulated insulin secretion tests | HOMA-IR, euglycemic clamp, insulin tolerance test |
| Impact in Diabetes | Reduced function leads to inadequate insulin secretion | Reduced sensitivity causes insulin resistance |
| Treatment Focus | Enhance beta-cell preservation and function | Improve insulin sensitivity via lifestyle or medication |
| Common Influencing Factors | Genetics, autoimmune damage, glucotoxicity | Obesity, physical inactivity, inflammation |
Introduction to Beta-Cell Function and Insulin Sensitivity
Beta-cell function refers to the ability of pancreatic beta cells to produce and secrete insulin in response to blood glucose levels. Insulin sensitivity describes how effectively the body's cells respond to insulin to facilitate glucose uptake. Together, these factors maintain glucose homeostasis and their impairment is central to the pathophysiology of type 2 diabetes.
Understanding Beta-Cell Physiology
Beta-cell function is crucial for regulating blood glucose levels by secreting insulin in response to rising glucose concentrations, directly impacting insulin sensitivity. Impaired beta-cell physiology, including reduced insulin secretion or abnormal cellular signaling, contributes to the pathogenesis of type 2 diabetes by failing to compensate for insulin resistance. Understanding the molecular mechanisms of beta-cell function, such as glucose sensing, insulin granule exocytosis, and the influence of incretins, is essential for developing targeted diabetes therapies.
Mechanisms of Insulin Sensitivity
Insulin sensitivity primarily depends on the efficient binding of insulin to its receptors on muscle, liver, and adipose cells, triggering a cascade that promotes glucose uptake and metabolism. Key mechanisms involve the activation of insulin receptor substrates (IRS), phosphatidylinositol 3-kinase (PI3K), and protein kinase B (Akt), which facilitate GLUT4 translocation to the cell membrane. Impairments in these signaling pathways contribute to insulin resistance, reducing glucose uptake and leading to metabolic dysregulation in beta-cell function.
Key Differences: Beta-Cell Function vs Insulin Sensitivity
Beta-cell function refers to the pancreas's ability to produce and secrete insulin in response to blood glucose levels, while insulin sensitivity describes how effectively the body's cells respond to insulin. Impaired beta-cell function results in inadequate insulin secretion, leading to hyperglycemia, whereas reduced insulin sensitivity, or insulin resistance, causes cells to respond poorly to insulin, increasing the demand on beta-cells. Both factors play crucial roles in glucose homeostasis and the pathogenesis of type 2 diabetes, but they differ fundamentally in their physiological mechanism and impact on metabolic health.
Interaction Between Beta-Cells and Insulin Action
Beta-cell function and insulin sensitivity are tightly interconnected in regulating glucose homeostasis, where beta-cells adjust insulin secretion to compensate for changes in insulin sensitivity. Impaired beta-cell function reduces the ability to produce adequate insulin in response to insulin resistance, leading to hyperglycemia and type 2 diabetes progression. The dynamic feedback loop between beta-cell responsiveness and peripheral insulin action is critical for maintaining metabolic balance and preventing glucose intolerance.
Clinical Assessment of Beta-Cell Function
Clinical assessment of beta-cell function primarily involves measuring insulin secretion in response to glucose stimuli, using tests such as the oral glucose tolerance test (OGTT) or hyperglycemic clamp technique. These evaluations are crucial for distinguishing between impaired beta-cell function and insulin resistance in conditions like type 2 diabetes. Accurate assessment of beta-cell function guides personalized treatment strategies and monitors disease progression effectively.
Evaluating Insulin Sensitivity in Practice
Evaluating insulin sensitivity in clinical practice primarily involves the use of indices derived from glucose and insulin measurements during oral glucose tolerance tests or fasting states, such as HOMA-IR and QUICKI. These tools quantitatively assess how effectively the body's cells respond to insulin, providing critical insights into metabolic health and the risk of type 2 diabetes. Accurate measurement of insulin sensitivity aids in distinguishing between beta-cell dysfunction and insulin resistance, guiding personalized treatment strategies.
Role in Type 2 Diabetes Pathogenesis
Beta-cell function and insulin sensitivity are critical determinants in the pathogenesis of Type 2 Diabetes. Impaired beta-cell function leads to inadequate insulin secretion, while reduced insulin sensitivity in peripheral tissues causes insulin resistance, jointly contributing to hyperglycemia. The interplay between declining beta-cell function and worsening insulin sensitivity accelerates disease progression and influences therapeutic strategies.
Therapeutic Strategies Targeting Beta-Cells and Insulin Sensitivity
Therapeutic strategies targeting beta-cells focus on preserving or enhancing beta-cell function through agents such as GLP-1 receptor agonists and DPP-4 inhibitors, which improve insulin secretion and reduce beta-cell stress. Insulin sensitivity is primarily addressed by medications like metformin and thiazolidinediones, which enhance peripheral glucose uptake and reduce hepatic glucose production. Combining therapies that target both beta-cell function and insulin sensitivity offers a comprehensive approach to managing type 2 diabetes by addressing core pathophysiological defects.
Future Directions in Diabetes Research
Advancing diabetes research increasingly targets the intricate interplay between beta-cell function and insulin sensitivity to develop precision therapies that restore glucose homeostasis. Emerging studies leverage genomics, artificial intelligence, and novel biomarkers to identify early impairments in beta-cell responsiveness and peripheral insulin action. Future directions emphasize personalized interventions and regenerative medicine approaches, aiming to preserve or enhance beta-cell mass alongside improving tissue-specific insulin sensitivity for effective diabetes management.
Beta-cell function Infographic
 libterm.com
libterm.com