Polypharmacy refers to the simultaneous use of multiple medications by a patient, often common among elderly individuals or those with chronic conditions. Managing polypharmacy effectively is crucial to minimize the risks of adverse drug interactions and side effects while ensuring optimal therapeutic outcomes. Explore this article to understand how You can recognize and safely navigate the challenges of polypharmacy.
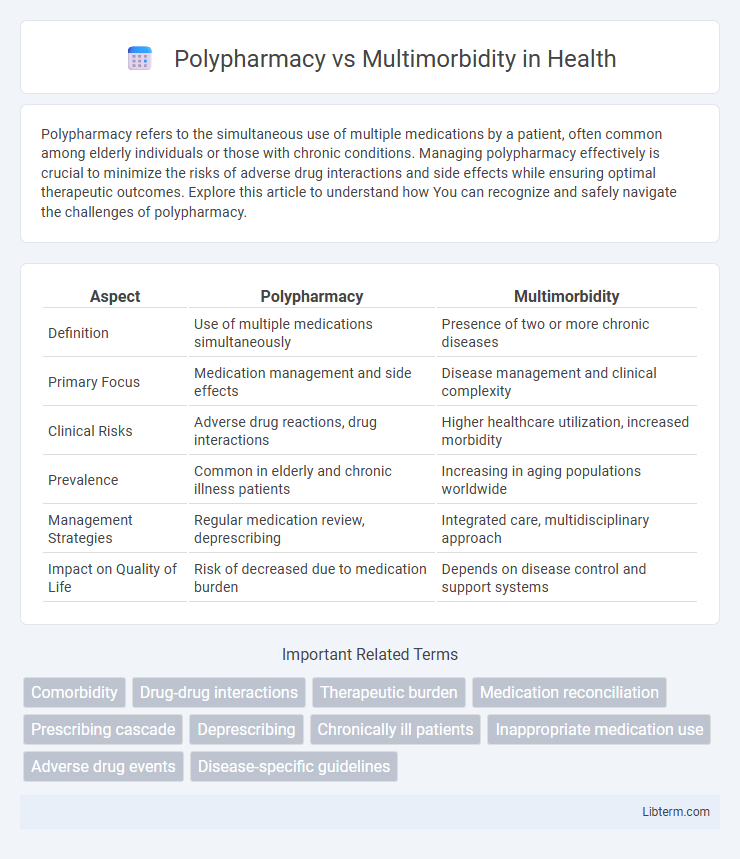
Table of Comparison
| Aspect | Polypharmacy | Multimorbidity |
|---|---|---|
| Definition | Use of multiple medications simultaneously | Presence of two or more chronic diseases |
| Primary Focus | Medication management and side effects | Disease management and clinical complexity |
| Clinical Risks | Adverse drug reactions, drug interactions | Higher healthcare utilization, increased morbidity |
| Prevalence | Common in elderly and chronic illness patients | Increasing in aging populations worldwide |
| Management Strategies | Regular medication review, deprescribing | Integrated care, multidisciplinary approach |
| Impact on Quality of Life | Risk of decreased due to medication burden | Depends on disease control and support systems |
Understanding Polypharmacy: Definition and Scope
Polypharmacy refers to the simultaneous use of multiple medications by a patient, typically defined as the intake of five or more drugs concurrently, which increases the risk of adverse drug reactions, drug interactions, and medication non-adherence. This concept differs from multimorbidity, which denotes the coexistence of two or more chronic conditions in an individual, often necessitating complex treatment regimens that contribute to polypharmacy. Understanding the scope of polypharmacy involves evaluating medication appropriateness, dose optimization, and careful monitoring to minimize harm while managing multimorbid patients effectively.
What Is Multimorbidity? Key Concepts Explained
Multimorbidity refers to the coexistence of two or more chronic diseases or conditions within a single individual, often complicating clinical management and treatment outcomes. It differs from polypharmacy, which specifically pertains to the use of multiple medications, often prescribed to manage multimorbidity but potentially leading to adverse drug interactions and side effects. Understanding multimorbidity is critical for developing personalized care plans that address complex health needs rather than isolated diseases.
The Link Between Polypharmacy and Multimorbidity
Polypharmacy, defined as the use of five or more medications concurrently, is commonly observed in patients with multimorbidity, which involves the coexistence of two or more chronic diseases. The complexity of managing multiple chronic conditions often necessitates prescribing multiple drugs, increasing the risk of adverse drug interactions and medication non-adherence. Effective management strategies must address both polypharmacy and multimorbidity to optimize patient outcomes and reduce healthcare costs.
Distinguishing Features: Polypharmacy vs Multimorbidity
Polypharmacy refers to the concurrent use of multiple medications by a patient, often defined as the intake of five or more drugs, primarily aimed at managing complex or multiple health conditions. Multimorbidity describes the coexistence of two or more chronic diseases or medical conditions within a single individual, regardless of the treatments involved. The key distinction lies in polypharmacy's focus on medication burden, while multimorbidity emphasizes the presence of multiple health disorders impacting patient care.
Risks and Challenges Associated with Polypharmacy
Polypharmacy significantly increases the risk of adverse drug reactions, medication non-adherence, and drug-drug interactions, particularly in elderly patients managing multiple chronic conditions. Challenges include difficulty in medication management, higher healthcare costs, and increased likelihood of hospitalizations due to drug-related complications. Effective strategies require comprehensive medication reviews and interprofessional collaboration to minimize risks and optimize treatment outcomes.
Managing Multimorbidity: Best Practices and Strategies
Managing multimorbidity requires a patient-centered approach that prioritizes comprehensive medication reviews to minimize polypharmacy-related risks such as adverse drug interactions and medication non-adherence. Integrating multidisciplinary care teams, including pharmacists, nurses, and specialists, enhances coordinated management plans tailored to individual patient needs and comorbid conditions. Utilizing evidence-based guidelines that consider the cumulative burden of multiple chronic diseases supports optimizing treatment efficacy while reducing redundancy and potential harm.
Clinical Implications of Polypharmacy in Multimorbid Patients
Polypharmacy in multimorbid patients significantly increases the risk of adverse drug reactions, medication non-adherence, and drug-drug interactions, complicating clinical management. Effective strategies involve comprehensive medication reviews, deprescribing where appropriate, and personalized treatment plans to balance therapeutic benefits and risks. Clinical monitoring and coordination among healthcare providers are essential to optimize outcomes and reduce hospitalizations related to polypharmacy complications.
Polypharmacy Prevention: Guidelines and Interventions
Polypharmacy prevention involves implementing evidence-based guidelines and targeted interventions to minimize unnecessary medication use, especially among older adults with multimorbidity. Strategies include regular medication reviews, deprescribing protocols, and patient-centered care plans to reduce adverse drug events and improve clinical outcomes. Clinical practice guidelines from organizations like the American Geriatrics Society emphasize comprehensive assessment and collaborative decision-making to optimize pharmacotherapy in complex patients.
Optimizing Patient Outcomes: Integrated Care Approaches
Optimizing patient outcomes amid polypharmacy and multimorbidity requires integrated care approaches that emphasize comprehensive medication review and individualized treatment plans. Coordinated interventions across multidisciplinary teams reduce adverse drug reactions and enhance adherence by aligning therapies with patients' complex health conditions. Utilizing electronic health records and decision support tools facilitates continuous monitoring and adjustment, promoting safer, more effective management of multiple chronic diseases.
Future Directions in Research on Polypharmacy and Multimorbidity
Future research on polypharmacy and multimorbidity prioritizes the development of precision medicine approaches to tailor medication regimens based on individual patient profiles and genetic markers. Innovative digital health technologies, including AI-driven clinical decision support systems, are being explored to optimize prescribing practices and minimize adverse drug interactions in complex multimorbid patients. Longitudinal studies are essential to evaluate the impact of deprescribing interventions and integrated care models on patient outcomes and healthcare costs over time.
Polypharmacy Infographic
 libterm.com
libterm.com