Chondromalacia involves the softening and breakdown of cartilage under the kneecap, causing knee pain and inflammation, while bursitis refers to the irritation and swelling of the fluid-filled sacs that cushion your joints. Both conditions can severely limit mobility and cause discomfort during everyday activities. Discover effective treatments and management strategies for these joint issues by reading the rest of the article.
Table of Comparison
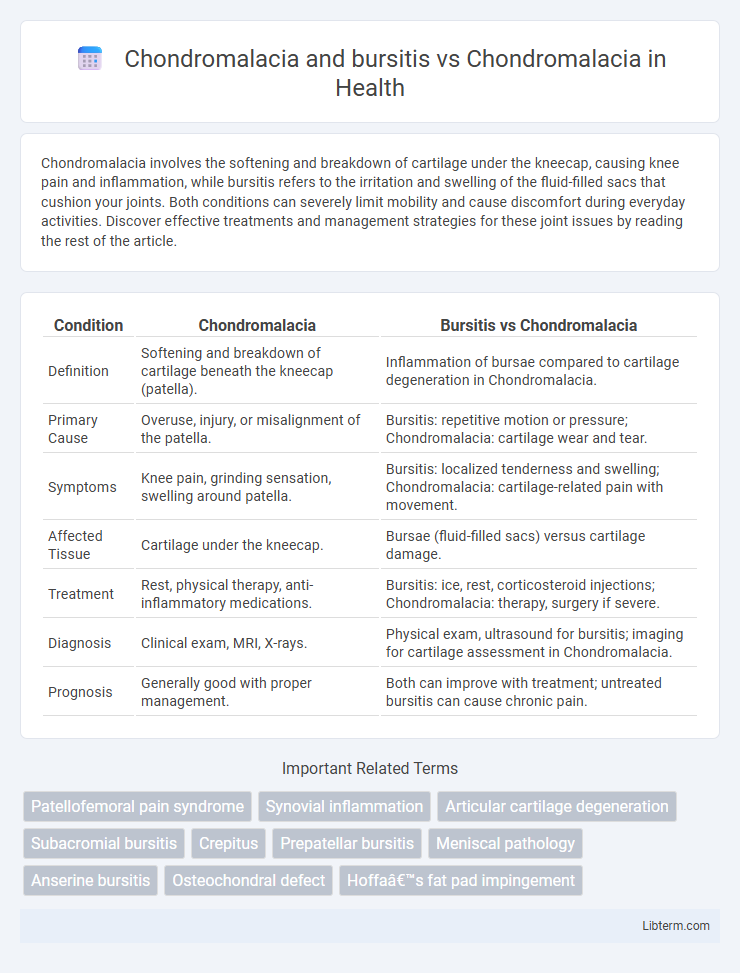
| Condition | Chondromalacia | Bursitis vs Chondromalacia |
|---|---|---|
| Definition | Softening and breakdown of cartilage beneath the kneecap (patella). | Inflammation of bursae compared to cartilage degeneration in Chondromalacia. |
| Primary Cause | Overuse, injury, or misalignment of the patella. | Bursitis: repetitive motion or pressure; Chondromalacia: cartilage wear and tear. |
| Symptoms | Knee pain, grinding sensation, swelling around patella. | Bursitis: localized tenderness and swelling; Chondromalacia: cartilage-related pain with movement. |
| Affected Tissue | Cartilage under the kneecap. | Bursae (fluid-filled sacs) versus cartilage damage. |
| Treatment | Rest, physical therapy, anti-inflammatory medications. | Bursitis: ice, rest, corticosteroid injections; Chondromalacia: therapy, surgery if severe. |
| Diagnosis | Clinical exam, MRI, X-rays. | Physical exam, ultrasound for bursitis; imaging for cartilage assessment in Chondromalacia. |
| Prognosis | Generally good with proper management. | Both can improve with treatment; untreated bursitis can cause chronic pain. |
Understanding Chondromalacia: Definition and Causes
Chondromalacia involves the softening and deterioration of the cartilage beneath the kneecap, primarily caused by injury, overuse, or misalignment of the knee joint. Bursitis, often occurring alongside chondromalacia, is the inflammation of bursae--small fluid-filled sacs that reduce friction between tissues--resulting from repetitive motion or direct trauma. Understanding the distinct causes and mechanisms of chondromalacia versus bursitis is crucial for accurate diagnosis and effective treatment strategies targeting cartilage degradation and inflammation respectively.
What is Bursitis? Key Differences from Chondromalacia
Bursitis is the inflammation of the bursae, small fluid-filled sacs that cushion bones, tendons, and muscles near joints, causing pain and swelling, primarily in areas like the knee, shoulder, or hip. Unlike chondromalacia, which involves the softening and deterioration of cartilage under the kneecap leading to joint pain and stiffness, bursitis results from repetitive motion or prolonged pressure and affects the bursae rather than the cartilage. Key differences include the source of pain--bursae inflammation in bursitis versus cartilage damage in chondromalacia--and treatment approaches focused on reducing inflammation for bursitis and cartilage repair or protection for chondromalacia.
Shared Symptoms of Chondromalacia and Bursitis
Chondromalacia and bursitis both commonly cause knee pain, swelling, and tenderness around the joint. Shared symptoms include a grinding or clicking sensation during knee movement and localized inflammation that exacerbates discomfort. These overlapping signs often complicate diagnosis, necessitating careful clinical evaluation and imaging for accurate differentiation.
Unique Signs: How Chondromalacia Stands Apart
Chondromalacia uniquely presents with a grating sensation and persistent anterior knee pain, particularly noticeable during activities like stair climbing or prolonged sitting, distinguishing it from bursitis, which primarily involves localized swelling and tenderness due to inflamed bursae. Unlike bursitis, chondromalacia involves cartilage softening and damage beneath the kneecap, leading to joint instability and a characteristic crepitus during knee movement. Diagnostic imaging such as MRI highlights cartilage degradation in chondromalacia, whereas bursitis typically shows fluid accumulation near the bursa, making clinical evaluation of pain location and movement sensitivity critical for differentiation.
Risk Factors: Who is Prone to Chondromalacia vs. Bursitis?
Chondromalacia primarily affects individuals with repetitive knee stress, such as athletes, runners, and those with structural knee abnormalities or muscle imbalances, while bursitis risk increases in people engaged in frequent kneeling, direct trauma, or systemic inflammatory conditions like rheumatoid arthritis. Age, overuse injuries, improper biomechanics, and previous knee injuries contribute significantly to chondromalacia development, whereas bursitis is often triggered by localized irritation or infection. Understanding these distinct risk profiles helps target prevention and tailored treatment for each condition.
Diagnosis: Distinguishing Chondromalacia from Bursitis
Diagnosis of chondromalacia centers on identifying cartilage softening and deterioration under the patella through MRI or arthroscopy, while bursitis diagnosis relies on detecting inflammation and fluid accumulation in bursae via physical examination and ultrasound imaging. Chondromalacia presents with anterior knee pain exacerbated by activities like climbing stairs, whereas bursitis often causes localized tenderness and swelling near the affected bursa. Differentiating these conditions is critical, as treatment varies: chondromalacia may require cartilage restoration strategies, while bursitis often responds to anti-inflammatory medications and rest.
Treatment Options: Chondromalacia Versus Bursitis
Treatment options for chondromalacia primarily involve physical therapy to strengthen the quadriceps muscles, NSAIDs for pain relief, and activity modification to reduce stress on the patella. Bursitis treatment focuses on reducing inflammation through corticosteroid injections, rest, ice application, and sometimes aspiration of the bursa fluid. Surgical intervention is rare for both conditions, reserved mainly for persistent cases unresponsive to conservative management.
Prevention Strategies for Both Conditions
Effective prevention strategies for chondromalacia and bursitis emphasize maintaining strong quadriceps muscles to support the knee joint and using proper techniques during physical activities to reduce joint stress. Incorporating regular stretching and low-impact exercises such as swimming or cycling can help improve joint flexibility and minimize inflammation around the patella. Avoiding repetitive knee trauma and ensuring adequate rest between workouts are essential to prevent the onset of both chondromalacia and bursitis.
Prognosis: Long-Term Outcomes in Chondromalacia and Bursitis
Chondromalacia combined with bursitis often leads to prolonged pain and swelling, complicating the recovery process compared to isolated chondromalacia. Long-term outcomes show that patients with both conditions are more likely to experience chronic discomfort, reduced joint function, and a higher risk of recurrent inflammation. Early intervention and targeted treatments improve prognosis, but persistent bursitis can delay full healing and increase the likelihood of surgery.
When to Seek Medical Advice for Knee Pain
Seek medical advice for knee pain when experiencing persistent discomfort, swelling, or reduced mobility, as these symptoms may indicate chondromalacia or bursitis requiring professional evaluation. Chondromalacia often causes a grinding sensation and pain under the kneecap, while bursitis presents with localized swelling and tenderness near the joint. Early diagnosis through imaging and physical examination helps prevent joint damage and promotes targeted treatment strategies.
Chondromalacia and bursitis Infographic
 libterm.com
libterm.com