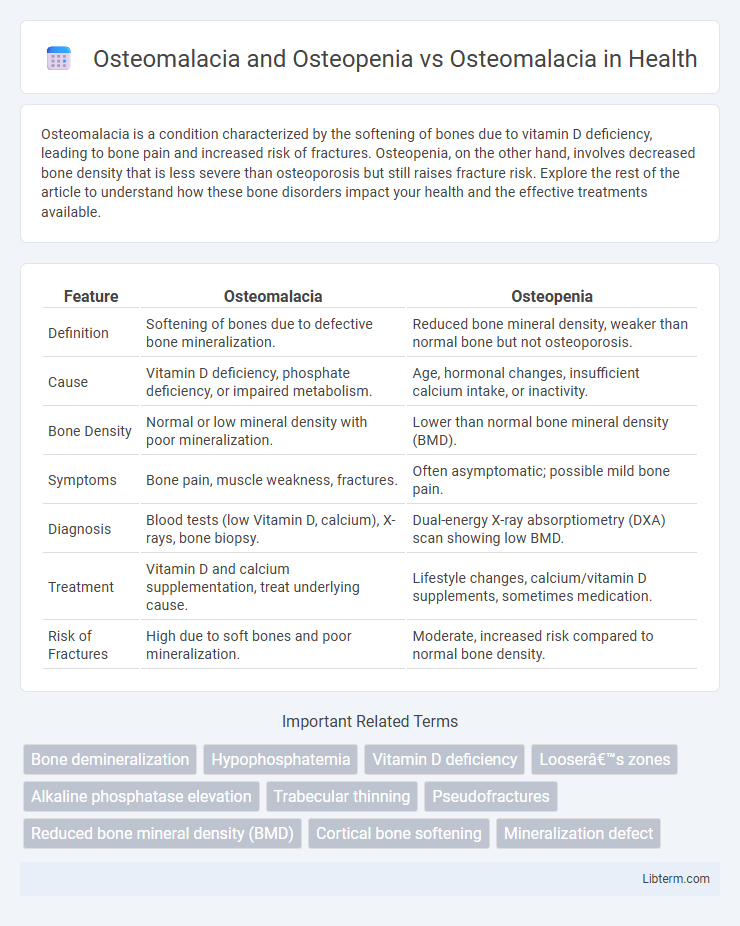
Osteomalacia is a condition characterized by the softening of bones due to vitamin D deficiency, leading to bone pain and increased risk of fractures. Osteopenia, on the other hand, involves decreased bone density that is less severe than osteoporosis but still raises fracture risk. Explore the rest of the article to understand how these bone disorders impact your health and the effective treatments available.
Table of Comparison
| Feature | Osteomalacia | Osteopenia |
|---|---|---|
| Definition | Softening of bones due to defective bone mineralization. | Reduced bone mineral density, weaker than normal bone but not osteoporosis. |
| Cause | Vitamin D deficiency, phosphate deficiency, or impaired metabolism. | Age, hormonal changes, insufficient calcium intake, or inactivity. |
| Bone Density | Normal or low mineral density with poor mineralization. | Lower than normal bone mineral density (BMD). |
| Symptoms | Bone pain, muscle weakness, fractures. | Often asymptomatic; possible mild bone pain. |
| Diagnosis | Blood tests (low Vitamin D, calcium), X-rays, bone biopsy. | Dual-energy X-ray absorptiometry (DXA) scan showing low BMD. |
| Treatment | Vitamin D and calcium supplementation, treat underlying cause. | Lifestyle changes, calcium/vitamin D supplements, sometimes medication. |
| Risk of Fractures | High due to soft bones and poor mineralization. | Moderate, increased risk compared to normal bone density. |
Understanding Osteomalacia: Causes and Symptoms
Osteomalacia is characterized by the softening of bones due to vitamin D deficiency, leading to impaired bone mineralization, distinct from osteopenia, which involves reduced bone density but not necessarily defective mineralization. Causes of osteomalacia include inadequate dietary vitamin D, malabsorption disorders, chronic kidney disease, and certain medications affecting vitamin D metabolism. Symptoms commonly manifest as diffuse bone pain, muscle weakness, and increased risk of fractures, necessitating early diagnosis and treatment to restore bone health.
What is Osteopenia? Definition and Risk Factors
Osteopenia is defined as a condition characterized by lower-than-normal bone mineral density, which is a precursor to osteoporosis and increases the risk of fractures. Risk factors for osteopenia include aging, hormonal changes such as reduced estrogen levels in postmenopausal women, inadequate calcium and vitamin D intake, sedentary lifestyle, and certain medications that affect bone metabolism. Unlike osteomalacia, which involves defective bone mineralization due to vitamin D deficiency, osteopenia primarily reflects decreased bone density without the softening of bones.
Osteomalacia vs Osteopenia: Key Differences
Osteomalacia is a metabolic bone disorder characterized by defective bone mineralization due to vitamin D deficiency, resulting in soft and weak bones. Osteopenia involves decreased bone mineral density but retains normal bone quality, often considered a precursor to osteoporosis. The key differences lie in osteomalacia's mineralization defect causing bone pain and fractures, while osteopenia mainly reflects reduced bone mass without compromising bone matrix.
How Osteomalacia Affects Bone Health
Osteomalacia significantly weakens bone health by causing defective bone mineralization, leading to soft and fragile bones prone to fractures and deformities. Unlike osteopenia, which involves reduced bone density but normal mineralization, osteomalacia results primarily from vitamin D deficiency or impaired phosphate metabolism, crucial for bone strength. This impaired mineralization disrupts the bone remodeling process, increasing the risk of skeletal pain and progressive bone weakening.
Diagnostic Approaches for Osteomalacia and Osteopenia
Diagnostic approaches for osteomalacia prioritize biochemical tests such as serum calcium, phosphate, alkaline phosphatase levels, and vitamin D deficiency detection, along with bone biopsy revealing unmineralized osteoid. Osteopenia diagnosis relies heavily on bone mineral density assessment through dual-energy X-ray absorptiometry (DEXA) scans to detect decreased bone mass without significant matrix abnormalities. Differentiating osteomalacia from osteopenia requires integrating laboratory results with imaging and clinical history to identify mineralization defects in osteomalacia versus reduced bone density in osteopenia.
Treatment Options for Osteomalacia
Treatment options for osteomalacia primarily focus on correcting vitamin D deficiency through high-dose vitamin D supplementation and adequate calcium intake, which helps restore normal bone mineralization. In contrast, osteopenia treatment often centers on lifestyle modifications such as weight-bearing exercises and nutritional support to prevent further bone loss. Monitoring and managing the underlying causes, such as malabsorption or chronic kidney disease, is essential in osteomalacia to ensure effective and sustained treatment results.
Managing Osteopenia: Prevention and Care
Managing osteopenia focuses on preventing bone loss through adequate calcium and vitamin D intake, regular weight-bearing exercise, and lifestyle modifications such as quitting smoking and limiting alcohol. Early diagnosis via bone density scanning allows for timely intervention to reduce fracture risk. Unlike osteomalacia, which results from defective bone mineralization due to vitamin D deficiency, osteopenia involves lower-than-normal bone density often preceding osteoporosis, necessitating proactive monitoring and care.
Overlapping Risk Factors: Osteomalacia and Osteopenia
Osteomalacia and osteopenia share overlapping risk factors such as vitamin D deficiency, inadequate calcium intake, and limited sunlight exposure, which impair bone mineralization and density respectively. Both conditions increase susceptibility to fractures due to weakened bone structure, especially in elderly populations or individuals with malabsorption syndromes. Addressing nutritional deficiencies and monitoring bone health through DXA scans are critical for early diagnosis and prevention of progression from osteopenia to more severe bone disorders like osteomalacia.
Diet and Lifestyle Changes for Bone Strength
Osteomalacia and osteopenia both involve weakened bones but differ in causes and pathology; osteomalacia results from vitamin D deficiency causing defective bone mineralization, while osteopenia is characterized by reduced bone density. Dietary improvements rich in vitamin D, calcium, and phosphorus are crucial for osteomalacia to enhance bone mineralization, whereas osteopenia management emphasizes sufficient calcium intake and weight-bearing exercise to preserve bone mass. Lifestyle changes such as increased sun exposure to boost endogenous vitamin D production and regular physical activity support bone strength and help prevent progression from osteopenia to osteoporosis.
Prognosis and Long-Term Outcomes in Osteomalacia and Osteopenia
Osteomalacia, characterized by defective bone mineralization due to vitamin D deficiency, often leads to bone pain and increased fracture risk, but responds well to appropriate treatment with vitamin D and calcium, resulting in favorable long-term outcomes. Osteopenia, defined by lower than normal bone mineral density without the mineralization defects seen in osteomalacia, carries a moderate risk of progression to osteoporosis and fractures if untreated, requiring lifestyle modification and risk factor management to improve prognosis. Distinguishing between osteomalacia and osteopenia is critical for prognosis since osteomalacia reverses with supplementation, while osteopenia requires ongoing monitoring to prevent deterioration and maintain bone health over time.
Osteomalacia and Osteopenia Infographic
 libterm.com
libterm.com