Contracture scars develop when skin tightens severely after a burn or injury, restricting movement and causing discomfort. These scars often affect joints and can limit your range of motion, which may require medical treatments like physical therapy or surgery to improve function. Explore the rest of the article to learn effective strategies for managing contracture scars and enhancing your recovery.
Table of Comparison
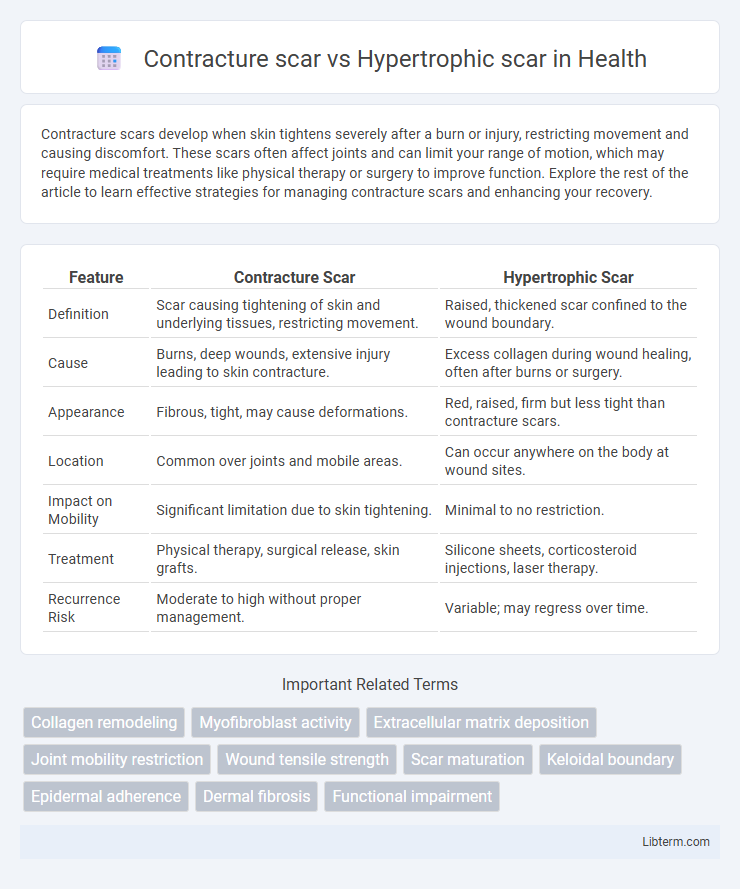
| Feature | Contracture Scar | Hypertrophic Scar |
|---|---|---|
| Definition | Scar causing tightening of skin and underlying tissues, restricting movement. | Raised, thickened scar confined to the wound boundary. |
| Cause | Burns, deep wounds, extensive injury leading to skin contracture. | Excess collagen during wound healing, often after burns or surgery. |
| Appearance | Fibrous, tight, may cause deformations. | Red, raised, firm but less tight than contracture scars. |
| Location | Common over joints and mobile areas. | Can occur anywhere on the body at wound sites. |
| Impact on Mobility | Significant limitation due to skin tightening. | Minimal to no restriction. |
| Treatment | Physical therapy, surgical release, skin grafts. | Silicone sheets, corticosteroid injections, laser therapy. |
| Recurrence Risk | Moderate to high without proper management. | Variable; may regress over time. |
Understanding Contracture Scars
Contracture scars occur when the skin and underlying tissues tighten, restricting movement and often resulting from deep burns or severe injury. These scars differ from hypertrophic scars by causing functional impairment due to tissue contraction, leading to limited mobility around joints. Effective treatment of contracture scars requires early intervention with physical therapy, splinting, or surgical release to restore range of motion and prevent permanent disability.
What Are Hypertrophic Scars?
Hypertrophic scars are raised, red scars that develop due to excessive collagen production during the wound healing process, typically confined within the original injury boundaries. Unlike contracture scars, which cause skin tightening and restrict movement, hypertrophic scars mainly result in thickened, firm tissue without significant functional impairment. These scars often improve over time and may respond to treatments such as silicone sheets, corticosteroid injections, or laser therapy.
Key Differences Between Contracture and Hypertrophic Scars
Contracture scars primarily restrict movement by tightening the skin and underlying tissues, often occurring after burns or deep wounds, whereas hypertrophic scars are raised, red scars that remain within the injury boundary without significant functional impairment. Contracture scars impair joint mobility due to tissue contraction, while hypertrophic scars mainly cause aesthetic concerns and may itch or thicken but do not typically restrict movement. Treatment approaches differ as contracture scars often require physical therapy and surgical intervention to restore function, whereas hypertrophic scars can be managed with silicone sheets, corticosteroid injections, or laser therapy.
Causes and Risk Factors
Contracture scars result from extensive skin and tissue damage that leads to tightening and restricted movement, often caused by deep burns or prolonged immobilization. Hypertrophic scars develop due to excessive collagen production during wound healing, frequently triggered by trauma, surgery, or infections. Risk factors for contracture scars include wound depth and location near joints, while hypertrophic scars are more common in individuals with darker skin tones or those with a genetic predisposition.
Clinical Appearance and Diagnosis
Contracture scars present clinically as tight, rigid areas restricting skin mobility, often resulting from burns or deep injuries, leading to functional impairment. Hypertrophic scars appear as raised, red, and thickened lesions confined within the original wound boundaries, typically appearing weeks after injury without causing contractures. Diagnosis relies on clinical examination assessing scar texture, color, extent, and functional limitations, with ultrasound or histopathology used to differentiate severe hypertrophic scars from keloids or contractures.
Functional Impact: Mobility and Cosmetic Concerns
Contracture scars significantly restrict mobility by causing tightness and deformity around joints, leading to impaired function and limited range of motion, whereas hypertrophic scars mainly cause cosmetic concerns with raised, red, and thickened tissue without severely affecting joint mobility. The contracture scar's impact on skin elasticity and underlying tissues often results in joint stiffness and difficulty performing daily activities, while hypertrophic scars may cause discomfort and itching but typically preserve functionality. Both scar types require targeted treatment, yet contracture scars demand more intensive interventions to restore movement and prevent long-term disability.
Common Treatment Options
Contracture scars often require physical therapy, silicone gel sheets, and sometimes surgical intervention like Z-plasty to restore mobility, while hypertrophic scars respond well to pressure therapy, corticosteroid injections, and laser treatments that reduce redness and thickness. Both types benefit from early wound care and silicone-based products to improve scar appearance and flexibility. Emerging treatments, such as laser therapy and platelet-rich plasma (PRP), show promise in enhancing scar remodeling for both contracture and hypertrophic scars.
Prevention Strategies for Scar Formation
Prevention strategies for contracture scars focus on early and consistent wound care, including pressure therapy, silicone gel sheets, and regular stretching exercises to maintain skin elasticity and prevent tissue tightening. Hypertrophic scars benefit from similar interventions such as silicone-based products, corticosteroid injections, and laser therapy to minimize collagen overproduction and reduce scar thickness. Both scar types require prompt treatment and monitoring to optimize healing outcomes and improve skin functionality.
Prognosis and Long-term Management
Contracture scars often lead to significant functional impairment due to tissue tightening, requiring aggressive physical therapy and sometimes surgical intervention to restore mobility. Hypertrophic scars, characterized by excessive collagen buildup within the wound boundary, typically improve with corticosteroid injections, silicone gel sheets, and laser therapy over time. Long-term management of contracture scars emphasizes preventing joint stiffness and maintaining range of motion, whereas hypertrophic scars demand ongoing monitoring for inflammation and symptomatic relief to minimize cosmetic concerns.
Frequently Asked Questions About Scar Types
Contracture scars often develop after burns, causing skin tightening that restricts movement, whereas hypertrophic scars are raised, red, and confined to the wound site without causing contracture. Patients frequently ask about the differences in treatment options; contracture scars may require physical therapy and surgical intervention, while hypertrophic scars are commonly managed with silicone sheets, corticosteroid injections, or laser therapy. Both scar types can benefit from early intervention, but contracture scars typically present more complex challenges due to their impact on mobility.
Contracture scar Infographic
 libterm.com
libterm.com