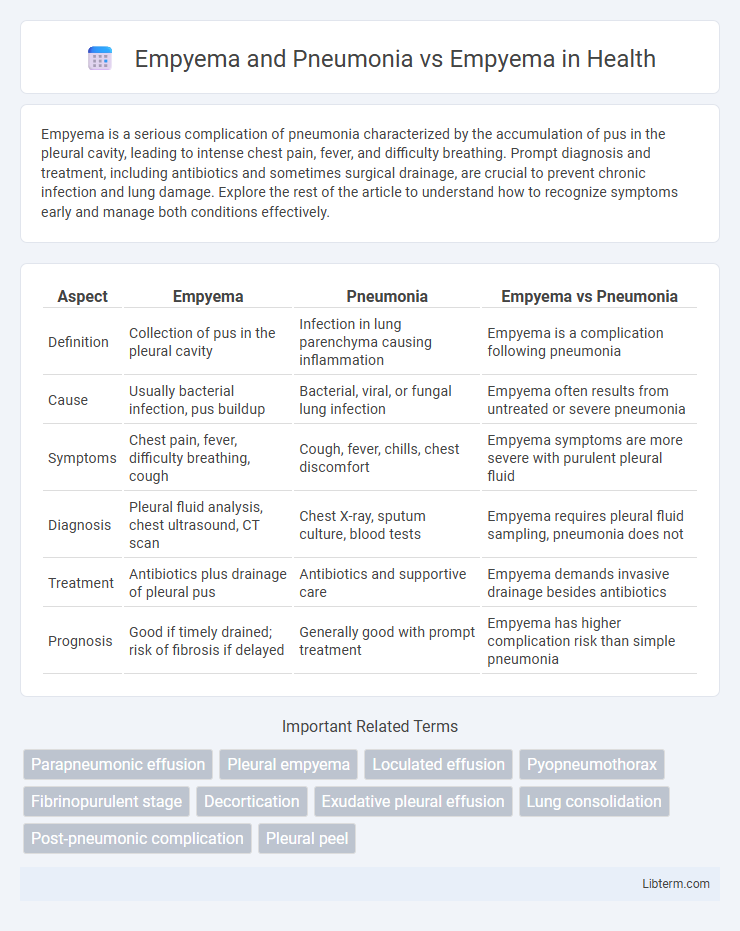
Empyema is a serious complication of pneumonia characterized by the accumulation of pus in the pleural cavity, leading to intense chest pain, fever, and difficulty breathing. Prompt diagnosis and treatment, including antibiotics and sometimes surgical drainage, are crucial to prevent chronic infection and lung damage. Explore the rest of the article to understand how to recognize symptoms early and manage both conditions effectively.
Table of Comparison
| Aspect | Empyema | Pneumonia | Empyema vs Pneumonia |
|---|---|---|---|
| Definition | Collection of pus in the pleural cavity | Infection in lung parenchyma causing inflammation | Empyema is a complication following pneumonia |
| Cause | Usually bacterial infection, pus buildup | Bacterial, viral, or fungal lung infection | Empyema often results from untreated or severe pneumonia |
| Symptoms | Chest pain, fever, difficulty breathing, cough | Cough, fever, chills, chest discomfort | Empyema symptoms are more severe with purulent pleural fluid |
| Diagnosis | Pleural fluid analysis, chest ultrasound, CT scan | Chest X-ray, sputum culture, blood tests | Empyema requires pleural fluid sampling, pneumonia does not |
| Treatment | Antibiotics plus drainage of pleural pus | Antibiotics and supportive care | Empyema demands invasive drainage besides antibiotics |
| Prognosis | Good if timely drained; risk of fibrosis if delayed | Generally good with prompt treatment | Empyema has higher complication risk than simple pneumonia |
Understanding Empyema: Definition and Causes
Empyema is a condition characterized by the accumulation of pus within the pleural cavity, often resulting from bacterial infections such as pneumonia. Pneumonia can lead to empyema when the infection spreads to the pleural space, causing inflammation and bacterial invasion that produces purulent fluid. Understanding empyema involves recognizing its causes, including untreated pneumonia, lung abscesses, or thoracic surgery complications, which contribute to the development of this serious pleural infection.
Pneumonia Overview: Types and Pathogenesis
Pneumonia, an acute respiratory infection, presents in multiple types including community-acquired, hospital-acquired, aspiration, and atypical pneumonia, each caused by diverse pathogens like bacteria, viruses, or fungi. The pathogenesis involves pathogen inhalation, colonization, and invasion of alveolar spaces, leading to inflammation, alveolar filling with exudate, and impaired gas exchange. Empyema, a complication of pneumonia, results from the accumulation of pus in the pleural cavity due to unresolved infection, distinguishing it from uncomplicated pneumonia by the presence of purulent pleural fluid and often requiring more intensive treatment.
Empyema vs Pneumonia: Key Differences
Empyema and pneumonia are related respiratory conditions but differ significantly in pathology; pneumonia is an infection causing inflammation in the lung parenchyma, while empyema involves the accumulation of purulent fluid in the pleural space. Empyema typically develops as a complication of untreated or severe pneumonia, characterized by the presence of thick pus and fibrous septations in the pleural cavity. Accurate differentiation is critical for treatment, as pneumonia primarily requires antibiotics whereas empyema often necessitates both antibiotic therapy and invasive drainage procedures.
How Pneumonia Can Lead to Empyema
Pneumonia, a lung infection caused by bacteria, viruses, or fungi, can lead to empyema when the infection progresses and pus accumulates in the pleural space. As bacteria invade the pleura, the body's immune response causes inflammation and fluid buildup, resulting in empyema, which complicates pneumonia. Prompt antibiotic treatment and drainage of the pleural fluid are critical to prevent severe complications and improve patient outcomes in cases where pneumonia leads to empyema.
Clinical Presentation: Symptoms Comparison
Empyema and pneumonia share common symptoms such as fever, cough, and chest pain, but empyema often presents with more severe pleuritic chest pain and persistent high fever despite antibiotic treatment. Patients with empyema may also exhibit decreased breath sounds and dullness to percussion on the affected side due to the accumulation of pus in the pleural space. Compared to pneumonia alone, empyema symptoms typically indicate a progression from lung infection to pleural involvement, resulting in worsened respiratory distress and systemic signs of infection.
Diagnostic Approaches for Empyema and Pneumonia
Empyema and pneumonia both require accurate diagnostic approaches to distinguish between the two conditions, as empyema involves the accumulation of pus in the pleural space, whereas pneumonia primarily affects lung parenchyma. Diagnostic tools include chest X-rays, which help detect pleural effusion suggestive of empyema, and thoracic ultrasound or CT scans, offering higher sensitivity for identifying pleural fluid collection and septations. Pleural fluid analysis through thoracentesis is essential for diagnosing empyema, assessing bacterial infection, and guiding targeted antibiotic therapy, while sputum cultures and blood tests aid in diagnosing pneumonia.
Imaging Findings: Radiological Distinctions
Empyema typically presents on imaging with a lenticular, loculated fluid collection in the pleural space, showing enhancement of the thickened pleural lining on contrast-enhanced CT scans. Pneumonia usually manifests as parenchymal consolidation with air bronchograms and no pleural effusion or with a simple effusion lacking septations or pleural thickening. Radiological distinctions include the presence of loculated fluid collections and pleural enhancement in empyema, which help differentiate it from the homogeneous lung infiltrates and potential non-loculated effusions seen in pneumonia.
Treatment Strategies: Empyema vs Pneumonia
Treatment strategies for empyema primarily involve drainage of pus through thoracentesis or chest tube insertion combined with targeted antibiotic therapy, whereas pneumonia treatment focuses on antimicrobial agents tailored to the causative pathogen without routine invasive drainage. Empyema often requires prolonged antibiotic courses and sometimes surgical intervention such as decortication when loculated pleural fluid impairs lung re-expansion. In pneumonia, supportive care including oxygen therapy and hydration is critical, while empyema management emphasizes removal of infected pleural fluid to prevent chronic complications.
Complications and Prognosis
Empyema, a collection of pus in the pleural cavity often resulting from pneumonia, carries complications such as lung fibrosis, bronchopleural fistula, and sepsis, which can worsen patient outcomes. Pneumonia complicated by empyema generally has a higher morbidity and prolonged recovery time compared to uncomplicated empyema, due to more extensive infection and inflammation. Prognosis depends heavily on timely drainage and appropriate antibiotic therapy, with delayed treatment increasing the risk of chronic lung impairment and mortality.
Prevention and Risk Reduction
Preventing pneumonia through vaccination against Streptococcus pneumoniae and influenza significantly reduces the risk of developing empyema, a severe complication characterized by pus accumulation in the pleural cavity. Early diagnosis and effective antibiotic treatment of pneumonia minimize bacterial spread, lowering the incidence of empyema. Maintaining good respiratory hygiene and managing chronic conditions such as diabetes and immunosuppression further decrease susceptibility to both pneumonia and its progression to empyema.
Empyema and Pneumonia Infographic
 libterm.com
libterm.com