Effective analgesia is crucial for managing pain during medical procedures and chronic conditions, improving patient comfort and overall quality of life. Various methods, including pharmacological treatments like opioids and non-opioid medications, as well as non-pharmacological approaches, target different pain pathways to provide relief. Explore the rest of this article to discover how tailored analgesic strategies can optimize Your pain management.
Table of Comparison
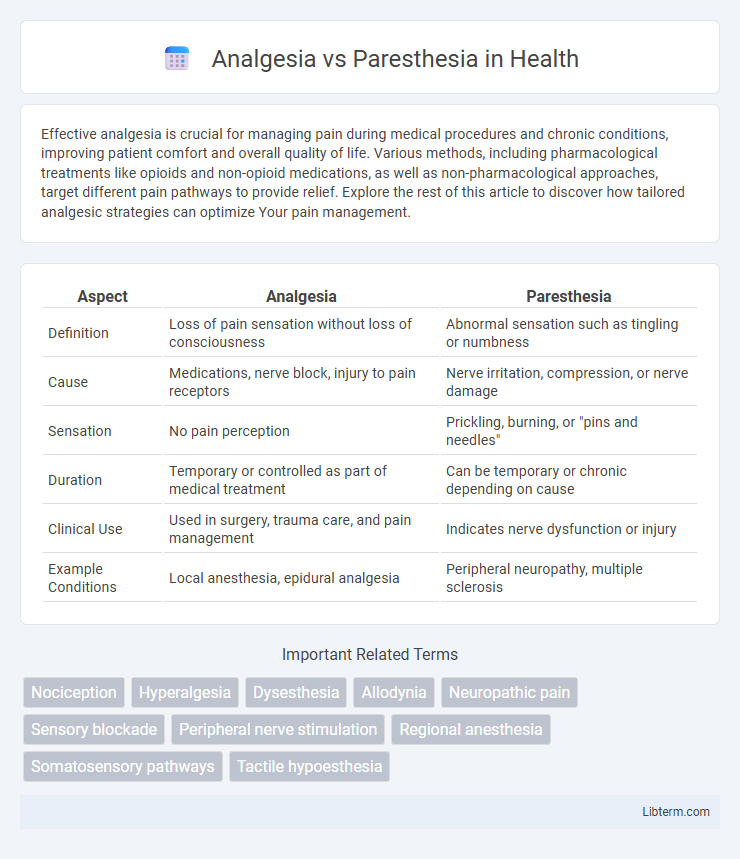
| Aspect | Analgesia | Paresthesia |
|---|---|---|
| Definition | Loss of pain sensation without loss of consciousness | Abnormal sensation such as tingling or numbness |
| Cause | Medications, nerve block, injury to pain receptors | Nerve irritation, compression, or nerve damage |
| Sensation | No pain perception | Prickling, burning, or "pins and needles" |
| Duration | Temporary or controlled as part of medical treatment | Can be temporary or chronic depending on cause |
| Clinical Use | Used in surgery, trauma care, and pain management | Indicates nerve dysfunction or injury |
| Example Conditions | Local anesthesia, epidural analgesia | Peripheral neuropathy, multiple sclerosis |
Introduction to Analgesia and Paresthesia
Analgesia refers to the absence of pain sensation while maintaining other sensory functions, commonly achieved through local anesthetics or systemic pain relief methods. Paresthesia describes abnormal sensations such as tingling, numbness, or prickling, often resulting from nerve damage, irritation, or compression. Understanding the distinction between analgesia and paresthesia is essential for accurate diagnosis and appropriate treatment of sensory disorders.
Defining Analgesia: Mechanisms and Effects
Analgesia refers to the loss of pain sensation without affecting other sensory modalities, achieved primarily through the inhibition of nociceptive signals in the peripheral or central nervous system. Mechanisms involve blocking pain receptors, reducing the release of neurotransmitters, or enhancing endogenous opioid pathways, effectively diminishing pain perception. The physiological effect of analgesia allows patients to experience pain relief while maintaining normal sensory and motor functions, distinguishing it from paresthesia which involves abnormal sensations like tingling or numbness.
Understanding Paresthesia: Causes and Symptoms
Paresthesia is characterized by abnormal sensations such as tingling, numbness, or burning, often caused by nerve compression, injury, or underlying medical conditions like diabetes and multiple sclerosis. Unlike analgesia, which refers to the absence of pain, paresthesia involves persistent sensory disturbances without necessarily impairing pain perception. Identifying the root cause of paresthesia is crucial for effective treatment and may involve diagnostic tests like nerve conduction studies or imaging to pinpoint nerve damage or dysfunction.
Key Differences Between Analgesia and Paresthesia
Analgesia refers to the absence of pain in response to stimuli that would normally be painful, resulting in numbness or a lack of sensation during medical procedures or nerve blocks. Paresthesia describes abnormal sensations such as tingling, prickling, or numbness, often indicating nerve irritation or damage without complete loss of sensation. Key differences include analgesia's role in pain elimination versus paresthesia's presentation as an uncomfortable or abnormal sensory experience.
Clinical Applications of Analgesia
Analgesia is primarily used in clinical settings to manage pain without affecting sensory perception, making it essential for procedures requiring patient comfort without complete numbness. Common applications include postoperative pain control, chronic pain management, and labor analgesia, where targeted pain relief improves patient outcomes and recovery times. Techniques such as peripheral nerve blocks, epidural analgesia, and systemic analgesics are favored for their ability to provide effective pain control while maintaining patient responsiveness.
Common Triggers and Risk Factors for Paresthesia
Paresthesia commonly arises from nerve compression, trauma, or systemic conditions such as diabetes and vitamin deficiencies, with repetitive motions and prolonged pressure on nerves being frequent triggers. Risk factors include previous nerve injury, underlying neurological disorders, and certain medications that affect nerve function. Analgesia differs by primarily involving the absence of pain sensation without the abnormal sensations characteristic of paresthesia.
Neurological Perspectives: Analgesia vs Paresthesia
Analgesia refers to the absence of pain perception caused by the inhibition of nociceptive pathways, often achieved through pharmacological agents targeting specific neural receptors such as opioid or sodium channels. Paresthesia involves abnormal sensations like tingling or numbness arising from aberrant neural signaling or nerve damage affecting peripheral or central nervous system pathways. Distinguishing these phenomena is crucial in neurology to optimize diagnostic accuracy and therapeutic interventions for neuropathic pain and sensory disorders.
Diagnostic Approaches for Sensory Disorders
Diagnostic approaches for sensory disorders differentiate analgesia, the absence of pain sensation, from paresthesia, characterized by abnormal sensations like tingling or numbness. Quantitative sensory testing (QST) and nerve conduction studies are essential tools, assessing sensory nerve function and distinguishing between loss of sensation and altered nerve activity. Imaging techniques such as MRI and skin biopsies provide structural and histological insights, facilitating accurate diagnosis of underlying neuropathies or central nervous system pathologies.
Treatment Strategies: Managing Analgesia and Paresthesia
Effective treatment strategies for managing analgesia focus on addressing the underlying cause of nerve dysfunction, often involving pharmacological interventions such as analgesics, anticonvulsants, or anti-inflammatory medications to reduce pain and improve nerve function. Paresthesia management typically involves symptomatic relief through medications like gabapentin or pregabalin, physical therapy, and lifestyle modifications to prevent nerve irritation or damage. Both conditions may require diagnostic evaluations, including nerve conduction studies or imaging, to tailor treatment plans and enhance patient outcomes.
Preventive Measures and Patient Education
Effective analgesia management requires patient education on medication adherence and potential side effects to prevent inadequate pain relief or complications. Preventive measures for paresthesia include careful nerve mapping and avoiding trauma during surgical or dental procedures, minimizing the risk of nerve injury. Emphasizing early symptom recognition and prompt reporting empowers patients to aid in timely intervention and improve outcomes.
Analgesia Infographic
 libterm.com
libterm.com