Neutrophilia is a condition characterized by an elevated number of neutrophils in the blood, often indicating an acute infection, inflammation, or stress response. This increase can also result from certain medications, bone marrow disorders, or chronic diseases, highlighting the importance of accurate diagnosis. Explore the article to understand the causes, symptoms, and treatment options to manage your health effectively.
Table of Comparison
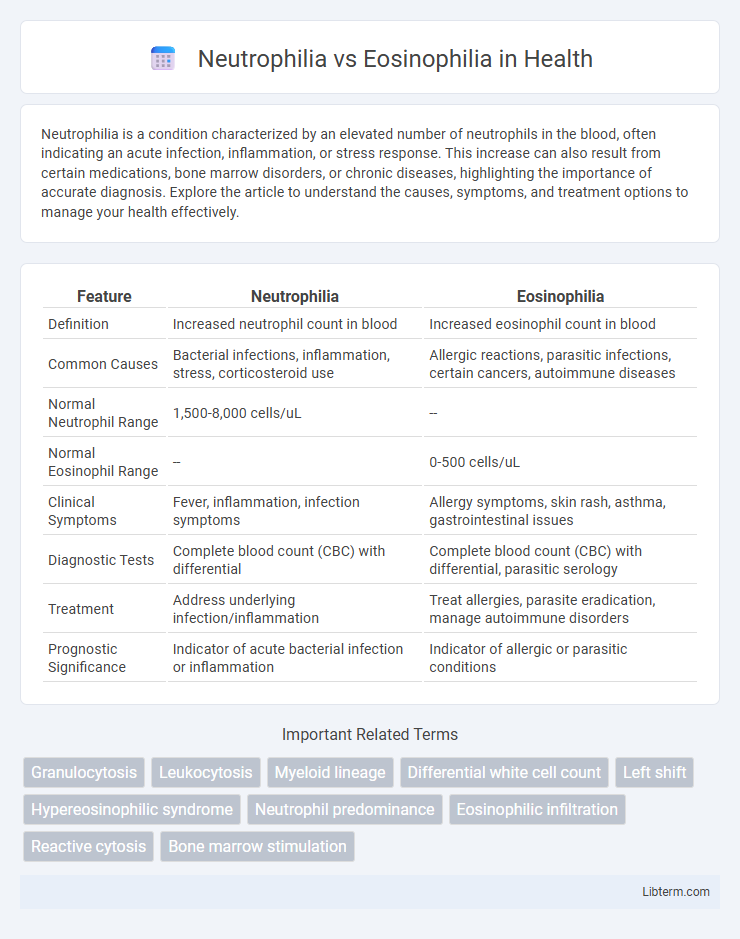
| Feature | Neutrophilia | Eosinophilia |
|---|---|---|
| Definition | Increased neutrophil count in blood | Increased eosinophil count in blood |
| Common Causes | Bacterial infections, inflammation, stress, corticosteroid use | Allergic reactions, parasitic infections, certain cancers, autoimmune diseases |
| Normal Neutrophil Range | 1,500-8,000 cells/uL | -- |
| Normal Eosinophil Range | -- | 0-500 cells/uL |
| Clinical Symptoms | Fever, inflammation, infection symptoms | Allergy symptoms, skin rash, asthma, gastrointestinal issues |
| Diagnostic Tests | Complete blood count (CBC) with differential | Complete blood count (CBC) with differential, parasitic serology |
| Treatment | Address underlying infection/inflammation | Treat allergies, parasite eradication, manage autoimmune disorders |
| Prognostic Significance | Indicator of acute bacterial infection or inflammation | Indicator of allergic or parasitic conditions |
Introduction to Neutrophilia and Eosinophilia
Neutrophilia is characterized by an elevated neutrophil count in the blood, often indicating bacterial infection, inflammation, or stress response. Eosinophilia involves an increased eosinophil count, commonly associated with allergic reactions, parasitic infections, and certain autoimmune diseases. Both conditions serve as important hematologic markers reflecting distinct underlying pathological processes.
Definition and Overview of Neutrophilia
Neutrophilia refers to an increased number of neutrophils in the blood, often exceeding 7,000 cells per microliter, typically indicating acute bacterial infections, inflammation, or stress responses. It is a common hematological condition characterized by the body's immune response mobilizing neutrophils to combat pathogens or tissue injury. In contrast, eosinophilia involves an elevated eosinophil count, usually linked to allergic reactions, parasitic infections, or certain autoimmune diseases.
Definition and Overview of Eosinophilia
Eosinophilia is characterized by an elevated eosinophil count in the blood, typically exceeding 500 cells per microliter, and is often associated with allergic reactions, parasitic infections, and certain autoimmune diseases. Unlike neutrophilia, which involves an increased number of neutrophils primarily due to bacterial infections or inflammation, eosinophilia specifically reflects immune responses to allergens or parasites. Identifying eosinophilia requires detailed blood tests and clinical correlation to determine underlying causes such as asthma, drug hypersensitivity, or eosinophilic disorders.
Causes of Neutrophilia
Neutrophilia primarily occurs due to bacterial infections, inflammation, stress responses, and certain medications like corticosteroids that stimulate neutrophil production. Other causes include acute tissue damage, such as burns or myocardial infarction, and hematologic disorders like chronic myeloid leukemia. Unlike eosinophilia, which is commonly associated with allergic reactions, parasitic infections, and autoimmune diseases, neutrophilia reflects an immediate innate immune response to tissue injury or infection.
Causes of Eosinophilia
Eosinophilia is primarily caused by allergic disorders such as asthma, hay fever, and drug hypersensitivity reactions, as well as parasitic infections like helminthiasis. Chronic inflammatory diseases, certain malignancies, and autoimmune conditions also contribute to elevated eosinophil levels. Unlike neutrophilia, which is often triggered by bacterial infections and acute inflammation, eosinophilia highlights immune responses related to allergens and parasites.
Clinical Manifestations: Comparing Symptoms
Neutrophilia presents with symptoms such as fever, signs of bacterial infection, and localized inflammation, often accompanied by increased white blood cell count and fatigue. Eosinophilia typically manifests with allergic reactions, asthma exacerbations, skin rashes, and gastrointestinal disturbances such as abdominal pain or diarrhea. Both conditions reflect underlying immune responses but differ significantly in their clinical presentations and associated diseases.
Diagnostic Criteria and Laboratory Findings
Neutrophilia is characterized by an elevated absolute neutrophil count above 7,500 cells/uL, often triggered by bacterial infections, inflammation, or stress response, with laboratory findings showing a left shift indicating increased band neutrophils. Eosinophilia is defined by an absolute eosinophil count exceeding 500 cells/uL, commonly associated with allergic reactions, parasitic infections, and certain hematologic disorders, with peripheral blood smears revealing increased eosinophil granules. Differentiation between neutrophilia and eosinophilia relies on automated complete blood count with differential and specific immunoassays to pinpoint the underlying etiology.
Underlying Pathophysiological Mechanisms
Neutrophilia is characterized by an elevated neutrophil count often due to acute bacterial infections, inflammation, or stress, driven by granulocyte colony-stimulating factor (G-CSF) that promotes neutrophil proliferation and mobilization from the bone marrow. Eosinophilia involves increased eosinophils commonly linked to allergic reactions, parasitic infections, or certain malignancies, mediated by interleukin-5 (IL-5) which stimulates eosinophil differentiation and activation. Both conditions reflect distinct immune response pathways, with neutrophilia primarily linked to innate immunity and acute inflammation, while eosinophilia is associated with adaptive immunity and hypersensitivity processes.
Treatment Approaches and Management Strategies
Neutrophilia treatment primarily involves addressing underlying infections or inflammatory conditions with antibiotics, corticosteroids, or immunosuppressive agents, depending on the cause. Eosinophilia management targets allergies, parasitic infections, or autoimmune diseases through antihistamines, corticosteroids, and antiparasitic medications. Both conditions require continuous monitoring of blood counts and symptom progression to tailor therapy effectively and prevent complications.
Key Differences Between Neutrophilia and Eosinophilia
Neutrophilia is characterized by an elevated neutrophil count, often indicating bacterial infections, inflammation, or stress responses, whereas eosinophilia involves increased eosinophil levels, commonly associated with allergic reactions, parasitic infections, and certain autoimmune diseases. Neutrophils primarily target bacteria and cellular debris, while eosinophils play a crucial role in combating parasites and modulating allergic inflammation. Laboratory findings differentiate these conditions by the dominant white blood cell type in a complete blood count with differential, guiding diagnostic and therapeutic approaches.
Neutrophilia Infographic
 libterm.com
libterm.com