Vasopressors are medications that constrict blood vessels and increase blood pressure, primarily used to treat severe hypotension in critical care settings. These drugs, such as norepinephrine and dopamine, support vital organ perfusion during shock or cardiac arrest. Discover how vasopressors work and their role in managing life-threatening conditions by reading the rest of the article.
Table of Comparison
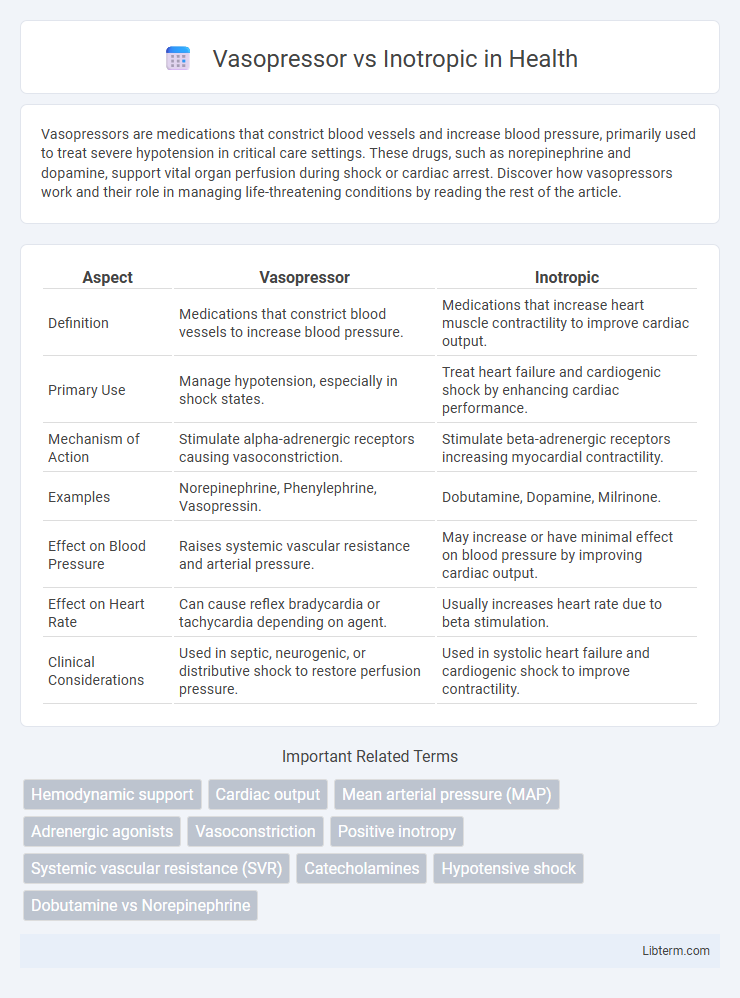
| Aspect | Vasopressor | Inotropic |
|---|---|---|
| Definition | Medications that constrict blood vessels to increase blood pressure. | Medications that increase heart muscle contractility to improve cardiac output. |
| Primary Use | Manage hypotension, especially in shock states. | Treat heart failure and cardiogenic shock by enhancing cardiac performance. |
| Mechanism of Action | Stimulate alpha-adrenergic receptors causing vasoconstriction. | Stimulate beta-adrenergic receptors increasing myocardial contractility. |
| Examples | Norepinephrine, Phenylephrine, Vasopressin. | Dobutamine, Dopamine, Milrinone. |
| Effect on Blood Pressure | Raises systemic vascular resistance and arterial pressure. | May increase or have minimal effect on blood pressure by improving cardiac output. |
| Effect on Heart Rate | Can cause reflex bradycardia or tachycardia depending on agent. | Usually increases heart rate due to beta stimulation. |
| Clinical Considerations | Used in septic, neurogenic, or distributive shock to restore perfusion pressure. | Used in systolic heart failure and cardiogenic shock to improve contractility. |
Introduction to Vasopressors and Inotropes
Vasopressors are medications that constrict blood vessels, raising blood pressure primarily by increasing systemic vascular resistance, crucial in managing hypotension during shock. Inotropes enhance cardiac contractility, improving cardiac output and oxygen delivery to tissues, often used in heart failure or cardiogenic shock. Both agents play vital roles in critical care, with vasopressors targeting vascular tone and inotropes focusing on myocardial function.
Definitions: What are Vasopressors and Inotropes?
Vasopressors are medications that constrict blood vessels, increasing vascular resistance and elevating blood pressure, primarily used in treating hypotension. Inotropes are drugs that enhance the force of cardiac muscle contractions, improving cardiac output without necessarily affecting vascular tone. Both agents play critical roles in managing circulatory shock but target different aspects of cardiovascular function.
Mechanism of Action: Vasopressors vs Inotropes
Vasopressors primarily act by stimulating alpha-adrenergic receptors, causing vasoconstriction that increases systemic vascular resistance and elevates blood pressure. Inotropes enhance myocardial contractility through beta-1 adrenergic receptor activation, improving cardiac output without significantly affecting vascular tone. Understanding these distinct mechanisms is crucial for targeted therapeutic intervention in conditions like septic shock and heart failure.
Clinical Indications for Vasopressors
Vasopressors are primarily indicated in clinical settings to manage hypotension and shock, especially septic, cardiogenic, and distributive shock, by constricting blood vessels and increasing systemic vascular resistance. These agents, such as norepinephrine and phenylephrine, are crucial for restoring adequate perfusion pressure in critically ill patients experiencing severe blood pressure drops. In contrast, inotropes like dobutamine are used mainly to enhance myocardial contractility rather than vascular tone.
Clinical Indications for Inotropes
Inotropes are primarily indicated in clinical scenarios involving heart failure with reduced ejection fraction, cardiogenic shock, and acute decompensated heart failure to enhance myocardial contractility and improve cardiac output. Unlike vasopressors, which mainly increase vascular tone and systemic vascular resistance, inotropes such as dobutamine, milrinone, and dopamine target myocardial contractile function. Clinical use of inotropes is essential in situations where cardiac pump failure results in inadequate tissue perfusion despite adequate preload and afterload management.
Key Differences: Vasopressors and Inotropes
Vasopressors primarily increase blood pressure by constricting blood vessels through alpha-adrenergic receptor stimulation, making them essential in treating hypotension and shock. Inotropes enhance myocardial contractility by acting on beta-adrenergic receptors, improving cardiac output without significantly affecting vascular tone. Understanding the key differences between vasopressors and inotropes guides precise clinical decisions in managing cardiovascular instability.
Common Examples of Vasopressors and Inotropes
Common examples of vasopressors include norepinephrine, epinephrine, and phenylephrine, which primarily act to increase vascular tone and elevate blood pressure. Inotropes such as dobutamine, milrinone, and dopamine enhance cardiac contractility, improving cardiac output without significantly affecting vascular resistance. The choice between vasopressors and inotropes depends on the clinical context, with vasopressors preferred for hypotension due to vasodilation and inotropes used in cases of cardiac pump failure.
Side Effects and Safety Concerns
Vasopressors, such as norepinephrine and phenylephrine, primarily increase blood pressure by vasoconstriction but carry risks like tissue ischemia, arrhythmias, and extravasation injuries. Inotropes, including dobutamine and milrinone, enhance myocardial contractility and can cause adverse effects such as tachycardia, arrhythmias, and increased myocardial oxygen consumption, leading to potential cardiac ischemia. Careful monitoring is essential for both drug classes due to their narrow therapeutic windows and risks of exacerbating underlying cardiovascular conditions.
Guidelines for Choosing Between Vasopressors and Inotropes
Guidelines for choosing between vasopressors and inotropes emphasize hemodynamic profiles, with vasopressors primarily used to increase systemic vascular resistance and blood pressure in hypotensive patients, while inotropes enhance cardiac contractility and cardiac output. Clinical indications include vasopressors such as norepinephrine for septic shock with vasodilation and inotropes like dobutamine for cardiogenic shock with low cardiac output. Hemodynamic monitoring and patient-specific factors, including blood pressure, cardiac function, and underlying etiology, guide optimal therapy selection based on current critical care protocols.
Summary and Clinical Implications
Vasopressors primarily act to increase vascular tone and elevate blood pressure by stimulating alpha-adrenergic receptors, making them essential in managing hypotension and septic shock. Inotropes enhance myocardial contractility through beta-adrenergic receptor activation, improving cardiac output in heart failure or cardiogenic shock. Clinically, selecting vasopressors or inotropes depends on hemodynamic goals; vasopressors are preferred to reverse vasodilatory shock, while inotropes target impaired cardiac contractile function, often necessitating careful monitoring to balance efficacy and adverse effects.
Vasopressor Infographic
 libterm.com
libterm.com