Calculus buildup on teeth is linked to inflammation that can affect blood vessels, potentially contributing to hypertension. Poor oral hygiene may increase systemic inflammation, exacerbating high blood pressure challenges. Explore the rest of the article to understand how your oral health impacts hypertension management.
Table of Comparison
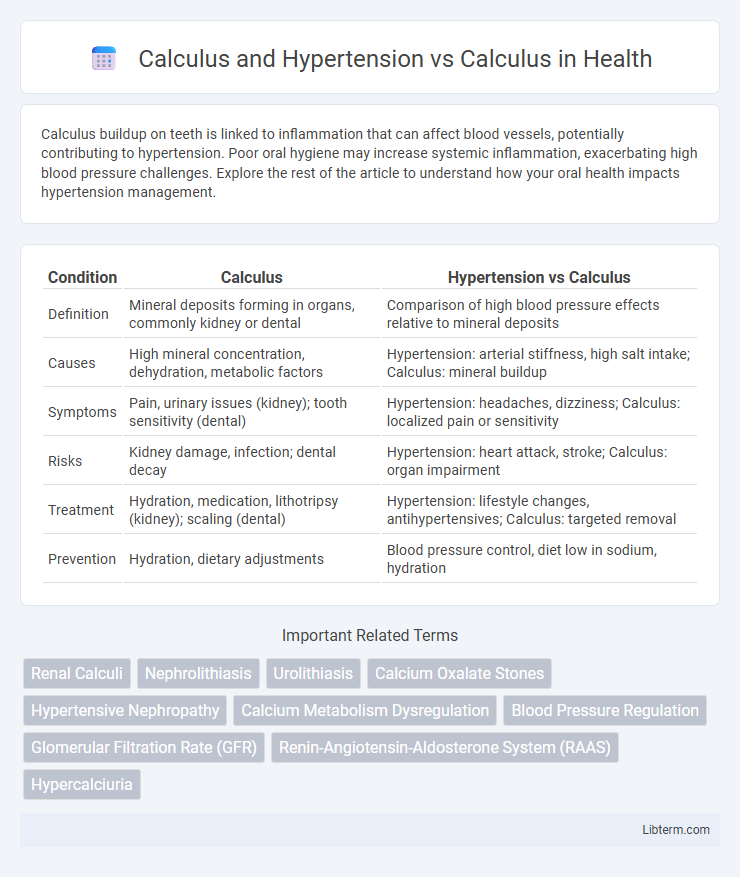
| Condition | Calculus | Hypertension vs Calculus |
|---|---|---|
| Definition | Mineral deposits forming in organs, commonly kidney or dental | Comparison of high blood pressure effects relative to mineral deposits |
| Causes | High mineral concentration, dehydration, metabolic factors | Hypertension: arterial stiffness, high salt intake; Calculus: mineral buildup |
| Symptoms | Pain, urinary issues (kidney); tooth sensitivity (dental) | Hypertension: headaches, dizziness; Calculus: localized pain or sensitivity |
| Risks | Kidney damage, infection; dental decay | Hypertension: heart attack, stroke; Calculus: organ impairment |
| Treatment | Hydration, medication, lithotripsy (kidney); scaling (dental) | Hypertension: lifestyle changes, antihypertensives; Calculus: targeted removal |
| Prevention | Hydration, dietary adjustments | Blood pressure control, diet low in sodium, hydration |
Introduction to Calculus and Hypertension
Calculus plays a crucial role in understanding hypertension by modeling blood flow dynamics and pressure variations within arteries. Mathematical equations derived from differential and integral calculus help analyze cardiovascular function and predict hypertension risk factors. This quantitative approach enables healthcare professionals to improve diagnosis and develop targeted treatment strategies for hypertension management.
Understanding Calculus: Definitions and Types
Calculus in mathematics involves the study of continuous change through differentiation and integration, fundamental for solving problems in physics and engineering. In contrast, calculus related to health refers to the formation of mineralized deposits, such as kidney or dental calculus, which can impact bodily functions and require medical attention. Understanding these distinct definitions and types is essential for correctly interpreting their applications in scientific and medical contexts.
Hypertension: Causes, Symptoms, and Risks
Hypertension, often referred to as high blood pressure, is a chronic medical condition where the force of blood against the artery walls is persistently elevated, increasing the risk of heart disease and stroke. Key causes include genetics, high sodium intake, obesity, stress, and lack of physical activity, while symptoms may be subtle, often described as headaches, shortness of breath, and nosebleeds in severe cases. Uncontrolled hypertension leads to serious complications such as kidney damage, vision loss, and aneurysms, making early detection and management critical for reducing overall cardiovascular risk.
The Link Between Calculus and Hypertension
Calcification in blood vessels, often referred to as vascular calculus, is strongly linked to hypertension due to arterial stiffness that increases systolic blood pressure. Studies show that calcium deposits in arterial walls contribute to reduced elasticity, leading to elevated hypertension risk and cardiovascular complications. Understanding this pathophysiological connection emphasizes the importance of managing calcium metabolism to prevent or mitigate hypertension-related vascular damage.
Pathophysiological Mechanisms Connecting Calculus and Hypertension
Calcification, or calculus formation, contributes to vascular stiffness through the deposition of calcium phosphate crystals in arterial walls, promoting hypertension by increasing systemic vascular resistance. This pathophysiological mechanism involves dysregulated calcium metabolism and inflammation, which induce endothelial dysfunction and impair vasodilation. The interplay between vascular calcification and elevated blood pressure results in a vicious cycle exacerbating arterial damage and promoting cardiovascular disease progression.
Calculus Management in Patients with Hypertension
Calculus management in patients with hypertension requires careful consideration of both cardiovascular and renal health to prevent stone formation and control blood pressure. Hypertensive patients often experience altered calcium metabolism, increasing the risk of nephrolithiasis, which necessitates tailored treatment plans involving dietary adjustments, pharmacologic interventions such as thiazide diuretics, and regular monitoring of serum electrolytes. Effective management integrates hypertension control and metabolic evaluation to reduce recurrence of urinary calculi and improve overall patient outcomes.
Diagnostic Approaches for Calculus with Hypertension
Diagnostic approaches for calculus with hypertension involve comprehensive evaluation combining imaging techniques like non-contrast CT scans to identify kidney stones and continuous blood pressure monitoring to assess hypertensive status. Laboratory tests including serum creatinine and electrolyte panels help evaluate renal function impacted by calculi, while ambulatory blood pressure monitoring aids in detecting hypertension patterns associated with urinary obstruction. Early and accurate diagnosis through these integrated methods is crucial in managing complications and tailoring effective treatment strategies for patients presenting with both calculus and hypertension.
Treatment Strategies: Calculus vs. Calculus with Hypertension
Treatment strategies for calculus alone emphasize pain management, hydration, and procedures such as extracorporeal shock wave lithotripsy (ESWL) or ureteroscopy to remove or break down kidney stones. In cases of calculus with hypertension, management includes not only stone removal but also strict blood pressure control through antihypertensive medications like ACE inhibitors or calcium channel blockers to reduce cardiovascular risk. Integrated care approaches address both urinary tract obstruction and systemic hypertension, improving patient outcomes and preventing recurrent complications.
Prevention Tips for Calculus and Hypertension
To prevent calculus, also known as kidney stones, drinking plenty of water helps dilute urine and reduce mineral crystal formation. Managing blood pressure through a balanced diet low in sodium and regular exercise lowers the risk of hypertension-related complications. Monitoring calcium intake and limiting foods high in oxalates can reduce the likelihood of both kidney stones and hypertension linked to impaired kidney function.
Future Research and Clinical Implications
Future research should explore the molecular mechanisms linking vascular calcification in hypertension to systemic calcium metabolism, aiming to identify novel therapeutic targets. Clinical implications include the potential development of personalized treatment strategies that address both hypertension and associated calcific vascular changes to reduce cardiovascular risks. Advancements in imaging and biomarker technologies will facilitate early detection and monitoring of calcification progression in hypertensive patients.
Calculus and Hypertension Infographic
 libterm.com
libterm.com