Progression is the continuous process of developing or advancing toward a more complete or improved state, often driven by consistent effort and strategic planning. Understanding how to measure and maintain progression can significantly impact your personal or professional growth. Explore this article to discover effective strategies for fostering unstoppable progression in your journey.
Table of Comparison
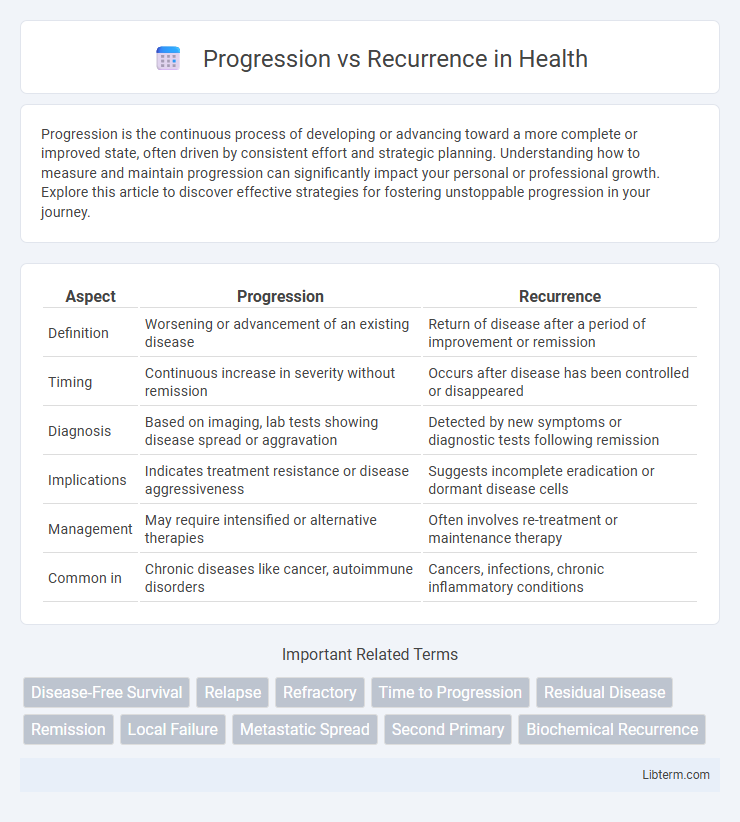
| Aspect | Progression | Recurrence |
|---|---|---|
| Definition | Worsening or advancement of an existing disease | Return of disease after a period of improvement or remission |
| Timing | Continuous increase in severity without remission | Occurs after disease has been controlled or disappeared |
| Diagnosis | Based on imaging, lab tests showing disease spread or aggravation | Detected by new symptoms or diagnostic tests following remission |
| Implications | Indicates treatment resistance or disease aggressiveness | Suggests incomplete eradication or dormant disease cells |
| Management | May require intensified or alternative therapies | Often involves re-treatment or maintenance therapy |
| Common in | Chronic diseases like cancer, autoimmune disorders | Cancers, infections, chronic inflammatory conditions |
Understanding Progression and Recurrence: Key Differences
Progression refers to the continual worsening or spread of a disease over time, often indicating an increase in severity or size of the original condition. Recurrence describes the return of a disease after a period of improvement or remission, typically manifesting in the same location or in a different part of the body. Understanding these distinctions is crucial for accurate diagnosis, treatment planning, and prognostic evaluation in clinical practice.
Defining Disease Progression
Disease progression refers to the worsening or advancement of a medical condition over time, characterized by an increase in severity, spread, or symptoms. It is typically measured through clinical assessments, imaging studies, or biomarker changes indicating growth or deterioration of the disease. Differentiating progression from recurrence is essential, as progression implies continuous disease activity, while recurrence indicates the return of disease after a period of remission.
What is Disease Recurrence?
Disease recurrence refers to the return of cancer or illness after a period of remission or apparent recovery, indicating that the disease was not entirely eradicated. It can manifest locally at the original site, regionally in nearby lymph nodes, or distantly in other organs, impacting treatment strategy and prognosis. Monitoring for recurrence involves regular follow-up exams, imaging, and biomarker tests to detect early signs and initiate timely intervention.
Clinical Markers of Progression vs Recurrence
Clinical markers of progression typically include increasing tumor size, new metastatic lesions on imaging, and rising tumor-specific biomarkers such as PSA in prostate cancer or CA-125 in ovarian cancer. Recurrence is often identified by the reappearance of symptoms or detectable disease after a period of remission, with markers such as rising carcinoembryonic antigen (CEA) in colorectal cancer or elevated thyroglobulin levels in thyroid cancer. Distinguishing progression from recurrence relies on timelines and patterns of marker changes, guiding treatment decisions and prognostic assessments.
Risk Factors Associated with Progression and Recurrence
Risk factors associated with progression include tumor grade, stage at diagnosis, and genetic mutations such as TP53 or EGFR alterations, which drive aggressive disease behavior. Recurrence risk is heightened by incomplete surgical resection, lymphovascular invasion, and the presence of residual microscopic disease. Both progression and recurrence correlate strongly with biomarkers like elevated Ki-67 index and changes in tumor microenvironment signaling pathways.
Diagnostic Approaches: Distinguishing Progression from Recurrence
Distinguishing progression from recurrence requires precise imaging techniques such as MRI with contrast enhancement and PET scans, which highlight metabolic activity differences between new tumor growth and residual disease. Molecular biomarkers and biopsy analyses provide critical data for identifying genetic mutations indicative of tumor evolution versus relapse. Advanced diagnostic algorithms integrating radiographic and molecular findings improve accuracy in differentiating true progression from treatment-related changes or pseudoprogression.
Treatment Strategies for Progression vs Recurrence
Treatment strategies for progression prioritize aggressive therapies such as targeted agents, immunotherapy, or combination regimens to halt disease advancement and improve survival outcomes. In contrast, recurrence management often involves salvage therapies, including localized interventions like surgery or radiation and systemic treatments tailored to prior response and resistance patterns. Precision medicine approaches leveraging genetic profiling optimize treatment selection to address biological differences between progression and recurrence.
Impact on Patient Prognosis
Progression of disease often indicates worsening tumor size or spread, leading to a poorer patient prognosis and reduced overall survival rates. Recurrence, particularly in aggressive cancers, signals the return of malignancy after treatment, frequently associated with more resistant disease and challenging management. Both progression and recurrence drastically influence treatment strategies and highlight the need for vigilant monitoring to improve patient outcomes.
Monitoring and Follow-up: Best Practices
Effective monitoring and follow-up for progression vs recurrence prioritize regular imaging and biomarker assessments tailored to the specific cancer type and stage. Clinical evaluations should emphasize symptom tracking and physical exams at defined intervals to detect changes promptly. Implementing standardized surveillance protocols based on evidence-based guidelines ensures timely identification and differentiation between progression and recurrence, optimizing patient outcomes.
Preventive Measures and Future Perspectives
Preventive measures for progression versus recurrence of disease emphasize early detection through regular screening, lifestyle modifications such as diet and exercise, and adherence to prescribed therapies to reduce risk factors. Emerging biomarkers and advanced imaging techniques offer promising future perspectives for personalized interventions that can distinguish progression from recurrence more accurately. Integration of artificial intelligence in patient monitoring holds potential to predict recurrence risks, enabling timely and tailored preventive strategies.
Progression Infographic
 libterm.com
libterm.com