Coagulation is the body's natural process to prevent excessive bleeding by forming blood clots, while anticoagulation therapy works to inhibit this process to prevent harmful clots from forming in blood vessels. Effective management of coagulation and anticoagulation is crucial in conditions like atrial fibrillation, deep vein thrombosis, and pulmonary embolism to balance the risk of bleeding and thrombosis. Explore the rest of this article to understand how these mechanisms work and what therapies might be best for your health.
Table of Comparison
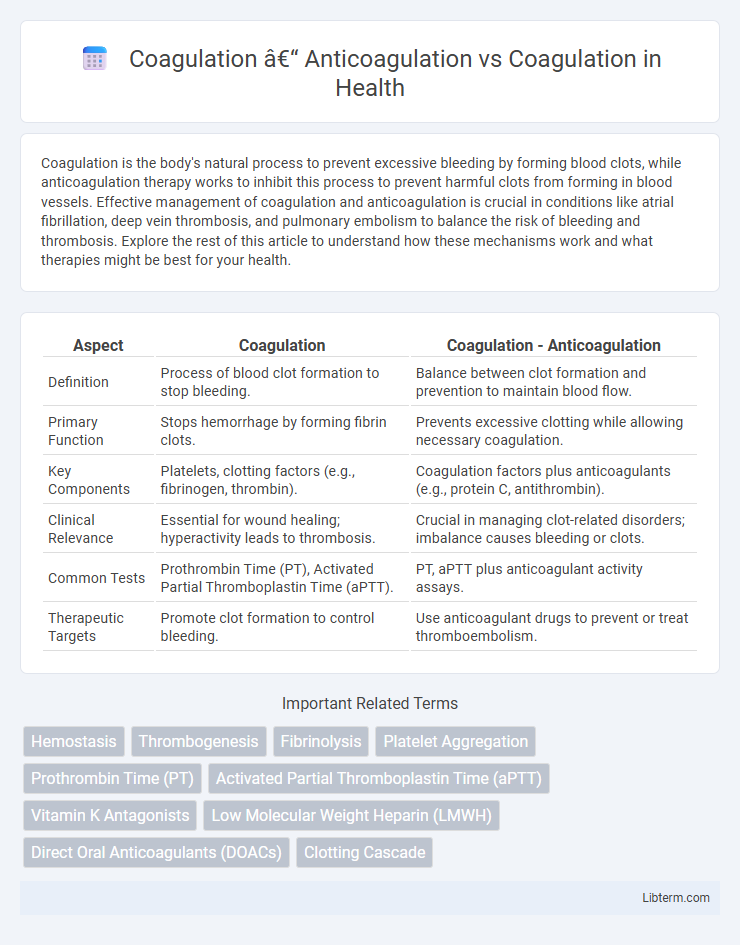
| Aspect | Coagulation | Coagulation - Anticoagulation |
|---|---|---|
| Definition | Process of blood clot formation to stop bleeding. | Balance between clot formation and prevention to maintain blood flow. |
| Primary Function | Stops hemorrhage by forming fibrin clots. | Prevents excessive clotting while allowing necessary coagulation. |
| Key Components | Platelets, clotting factors (e.g., fibrinogen, thrombin). | Coagulation factors plus anticoagulants (e.g., protein C, antithrombin). |
| Clinical Relevance | Essential for wound healing; hyperactivity leads to thrombosis. | Crucial in managing clot-related disorders; imbalance causes bleeding or clots. |
| Common Tests | Prothrombin Time (PT), Activated Partial Thromboplastin Time (aPTT). | PT, aPTT plus anticoagulant activity assays. |
| Therapeutic Targets | Promote clot formation to control bleeding. | Use anticoagulant drugs to prevent or treat thromboembolism. |
Introduction to Coagulation
Coagulation is a critical physiological process where blood transforms from a liquid to a gel, forming clots that prevent excessive bleeding upon vascular injury. This complex cascade involves platelets, clotting factors such as fibrinogen, and proteins like thrombin working synergistically to stabilize the wound site. Understanding coagulation is essential for distinguishing between normal clot formation and pathological conditions requiring anticoagulation therapy to prevent thrombosis.
The Physiology of Blood Coagulation
The physiology of blood coagulation involves a complex cascade of enzymatic reactions that lead to the transformation of fibrinogen into fibrin, stabilizing the blood clot. Anticoagulation mechanisms regulate this process by inhibiting key factors such as thrombin and factor Xa to prevent excessive clot formation, maintaining vascular integrity. Understanding the balance between coagulation and anticoagulation is critical for managing disorders like thrombosis and hemorrhage.
Key Factors Involved in Coagulation
Key factors involved in coagulation include clotting factors such as fibrinogen, prothrombin, and factors VII, VIII, IX, and X, which work in a complex cascade to form a stable fibrin clot. Platelets play a crucial role by adhering to damaged blood vessels and providing a surface for clotting factor activation. Anticoagulation mechanisms involve proteins like antithrombin III, protein C, and protein S, which regulate coagulation to prevent excessive clot formation and maintain vascular health.
What Is Anticoagulation?
Anticoagulation refers to the process of preventing blood clot formation by inhibiting the coagulation cascade through medications such as warfarin, heparin, and direct oral anticoagulants (DOACs). It is essential in managing conditions like deep vein thrombosis (DVT), atrial fibrillation, and pulmonary embolism to reduce the risk of stroke and other thromboembolic events. Anticoagulation therapy balances the risk of clot formation with the potential for bleeding complications, necessitating careful monitoring and dosage adjustments.
Mechanisms of Anticoagulant Action
Anticoagulants inhibit blood clot formation by targeting specific factors within the coagulation cascade, such as thrombin or factor Xa, preventing fibrin generation essential for clot stabilization. Heparin enhances antithrombin III activity, accelerating the inactivation of thrombin and factor Xa, while warfarin inhibits vitamin K-dependent synthesis of clotting factors II, VII, IX, and X. Direct oral anticoagulants (DOACs) selectively block active sites of thrombin or factor Xa, providing targeted anticoagulation without affecting upstream coagulation pathways.
Clinical Indications for Anticoagulation
Anticoagulation therapy is primarily indicated for preventing thromboembolic events in conditions such as atrial fibrillation, deep vein thrombosis (DVT), pulmonary embolism (PE), and mechanical heart valve replacement. It is essential for reducing stroke risk in patients with non-valvular atrial fibrillation and for managing acute and chronic venous thromboembolism episodes. Careful clinical assessment determines the balance between preventing clot formation and minimizing bleeding risks during anticoagulation management.
Comparing Anticoagulation vs Coagulation
Coagulation is the physiological process where blood transforms from a liquid to a gel, forming clots to prevent excessive bleeding, primarily involving fibrin and platelets. Anticoagulation refers to the inhibition or delay of this clotting process, achieved through agents such as heparin, warfarin, or direct oral anticoagulants (DOACs), which target specific factors in the coagulation cascade. While coagulation promotes hemostasis and tissue repair, anticoagulation is critical in preventing pathological thrombosis that can lead to conditions like stroke, deep vein thrombosis, or pulmonary embolism.
Risks and Complications of Coagulation and Anticoagulation
Coagulation is essential for stopping bleeding but carries risks such as thrombosis and embolism when dysregulated, leading to complications like stroke or deep vein thrombosis. Anticoagulation therapy reduces these risks by preventing clot formation but increases the probability of bleeding complications, including hemorrhage and intracranial bleeding. Balancing coagulation and anticoagulation is critical to minimize adverse events while managing conditions such as atrial fibrillation, venous thromboembolism, or mechanical heart valves.
Monitoring and Managing Coagulation Status
Monitoring coagulation status involves assessing parameters such as prothrombin time (PT), activated partial thromboplastin time (aPTT), and international normalized ratio (INR) to evaluate blood clotting efficiency and anticoagulation therapy effectiveness. Managing coagulation requires tailored adjustments of anticoagulant dosing, including warfarin, heparin, or direct oral anticoagulants (DOACs), based on continuous laboratory results and patient-specific risk factors for thrombosis and bleeding. Point-of-care testing and frequent monitoring improve therapeutic outcomes by balancing coagulation and anticoagulation, minimizing complications in disorders like deep vein thrombosis (DVT) or atrial fibrillation (AF).
Future Perspectives in Coagulation Therapy
Future perspectives in coagulation therapy emphasize the development of targeted anticoagulants with enhanced safety profiles and personalized medicine approaches using genetic and biomarker analysis to optimize treatment efficacy. Innovations in nanotechnology and drug delivery systems aim to improve the precision of anticoagulant dosing while minimizing bleeding risks. Research on novel anticoagulant agents and point-of-care diagnostic tools continues to transform management strategies for thrombotic disorders and bleeding complications.
Coagulation – Anticoagulation Infographic
 libterm.com
libterm.com