Corticosteroids are powerful medications commonly used to reduce inflammation and suppress the immune response in various conditions such as asthma, arthritis, and allergic reactions. These drugs work by mimicking the effects of hormones produced naturally by your adrenal glands, helping to manage symptoms effectively. Explore the rest of the article to learn more about how corticosteroids might benefit your treatment plan and their potential side effects.
Table of Comparison
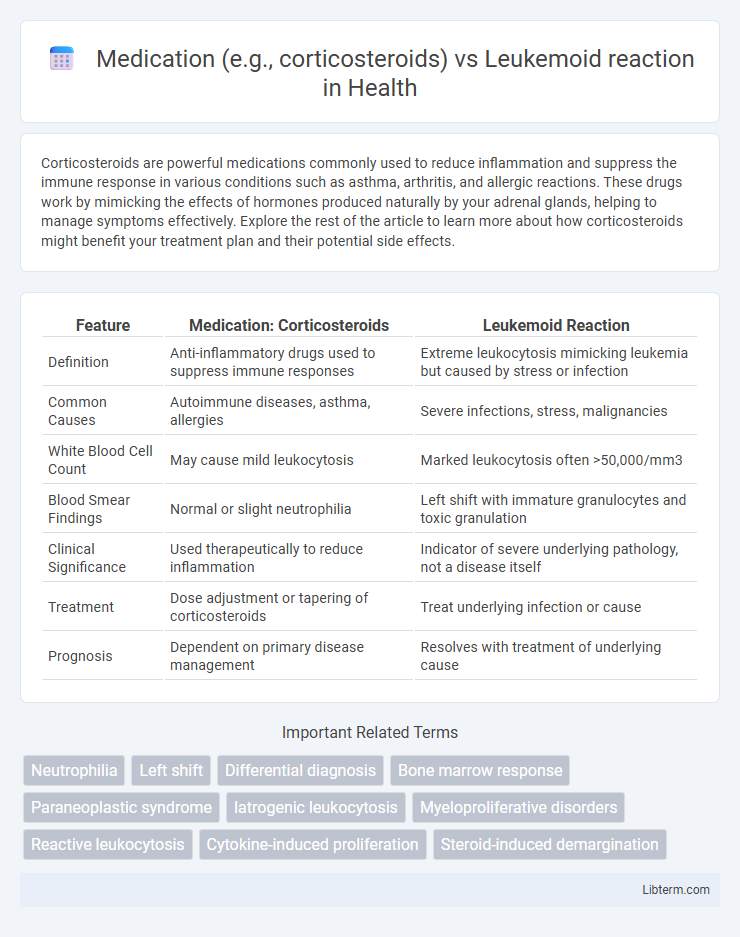
| Feature | Medication: Corticosteroids | Leukemoid Reaction |
|---|---|---|
| Definition | Anti-inflammatory drugs used to suppress immune responses | Extreme leukocytosis mimicking leukemia but caused by stress or infection |
| Common Causes | Autoimmune diseases, asthma, allergies | Severe infections, stress, malignancies |
| White Blood Cell Count | May cause mild leukocytosis | Marked leukocytosis often >50,000/mm3 |
| Blood Smear Findings | Normal or slight neutrophilia | Left shift with immature granulocytes and toxic granulation |
| Clinical Significance | Used therapeutically to reduce inflammation | Indicator of severe underlying pathology, not a disease itself |
| Treatment | Dose adjustment or tapering of corticosteroids | Treat underlying infection or cause |
| Prognosis | Dependent on primary disease management | Resolves with treatment of underlying cause |
Introduction: Understanding Leukemoid Reactions
Leukemoid reactions represent an extreme reactive leukocytosis, often mimicking leukemia but caused by infections, stress, or medications like corticosteroids. Corticosteroids induce demargination of neutrophils, leading to elevated white blood cell counts that can complicate the differential diagnosis. Recognizing the distinction between corticosteroid-induced leukocytosis and leukemoid reactions is critical for accurate clinical assessment and treatment planning.
Defining Leukemoid Reactions and Their Causes
Leukemoid reactions are characterized by an extreme elevation in white blood cell count, often resembling leukemia but caused by an underlying condition such as severe infection or inflammation. Unlike corticosteroids, which can induce leukocytosis by releasing neutrophils from the bone marrow, leukemoid reactions are a reactive process triggered by factors like toxins, malignancies, or stress. Identifying the cause involves differentiating between drug-induced leukocytosis and pathological responses, with leukemoid reactions typically presenting with a marked leukocyte alkaline phosphatase score and an absence of the Philadelphia chromosome.
Medication-Induced Leukemoid Reactions: An Overview
Medication-induced leukemoid reactions often occur as a side effect of corticosteroids, which can cause a significant increase in white blood cell counts mimicking leukemia. These reactions are characterized by a reversible leukocytosis, predominantly neutrophilia, following drug administration, with corticosteroids altering the demargination and release of white blood cells from the bone marrow. Recognizing medication-induced leukemoid reactions prevents misdiagnosis and unnecessary treatment, emphasizing the importance of thorough patient medication history in clinical evaluations.
Corticosteroids and Their Hematologic Effects
Corticosteroids induce significant hematologic changes, such as leukocytosis characterized by neutrophilia due to demargination of neutrophils and reduced lymphocyte counts through redistribution and apoptosis. This steroid-induced leukocytosis can mimic a leukemoid reaction, complicating differential diagnosis in patients with infections or inflammatory conditions. Understanding corticosteroids' effects on white blood cell dynamics is essential for accurate interpretation of complete blood counts and avoiding misdiagnosis.
Mechanisms of Action: Medications vs Leukemoid Pathophysiology
Corticosteroids modulate leukemoid reaction primarily by suppressing the immune response and reducing systemic inflammation, which consequently lowers the excessive white blood cell production characteristic of leukemoid reactions. The leukemoid reaction involves an exaggerated bone marrow response to severe infections or stress, leading to a marked leukocytosis that mimics leukemia but is reactive rather than neoplastic. Mechanistically, corticosteroids downregulate cytokine production and inflammatory mediators, while the leukemoid reaction pathophysiology is driven by heightened granulocyte colony-stimulating factor (G-CSF) and interleukin signaling stimulating myeloid proliferation.
Diagnostic Challenges: Differentiating Leukemoid Reaction from Leukemia
Distinguishing a leukemoid reaction from leukemia poses significant diagnostic challenges due to overlapping clinical features such as elevated white blood cell counts and the presence of immature myeloid cells. Corticosteroid medication can exacerbate leukocytosis, mimicking leukemia and complicating differential diagnosis through peripheral blood smear and bone marrow examination. Advanced molecular testing, including cytogenetics and flow cytometry, is essential to accurately differentiate reactive leukemoid processes from malignant hematologic diseases.
Clinical Presentation and Lab Findings
Corticosteroid administration can induce leukocytosis characterized by elevated neutrophil counts without a left shift, often mimicking a leukemoid reaction, which presents with marked leukocytosis and a left shift including immature granulocytes such as myelocytes and metamyelocytes. Clinically, leukemoid reactions are frequently associated with underlying infections or malignancies, whereas corticosteroid-induced leukocytosis typically lacks systemic symptoms. Laboratory findings in leukemoid reaction include elevated leukocyte alkaline phosphatase (LAP) scores, contrasting with normal or decreased LAP scores in chronic myeloid leukemia, and corticosteroid use generally does not alter LAP scores but increases neutrophil demargination and bone marrow release.
Management Strategies for Medication-Induced Leukemoid Reactions
Management of medication-induced leukemoid reactions, particularly those triggered by corticosteroids, involves immediate cessation or dose reduction of the offending drug to prevent exacerbation of leukocytosis. Supportive care includes monitoring white blood cell counts and addressing any underlying infections or complications associated with the leukemoid reaction. In severe cases, corticosteroid tapering protocols and alternative immunosuppressive therapies may be implemented to balance treatment efficacy with hematologic safety.
Prognosis and Complications
Corticosteroid use can induce a leukemoid reaction, characterized by an extreme elevation of white blood cells mimicking leukemia but typically with a favorable prognosis when the underlying cause is addressed. Prognosis improves with timely identification and discontinuation of the medication, as the leukemoid reaction is usually reversible without long-term complications. Complications arise primarily if the leukemoid reaction is mistaken for malignant conditions, leading to unnecessary aggressive treatments and delayed appropriate care.
Conclusion: Key Takeaways on Medication vs Leukemoid Reactions
Corticosteroids and other medications can induce leukemoid reactions by stimulating white blood cell production, mimicking leukemia but resulting from non-malignant causes. Recognizing medication-induced leukemoid reactions is crucial for accurate diagnosis and avoiding unnecessary treatments for malignancy. Close monitoring of medication history and white blood cell counts ensures differentiation between leukemoid reactions and hematologic disorders.
Medication (e.g., corticosteroids) Infographic
 libterm.com
libterm.com