Meningitis is a serious inflammation of the membranes surrounding the brain and spinal cord, often caused by infections from bacteria, viruses, or fungi. Early symptoms include fever, headache, neck stiffness, and sensitivity to light, which require prompt medical attention to prevent severe complications. Discover more about how meningitis affects your body, symptoms to watch for, and treatment options in the full article.
Table of Comparison
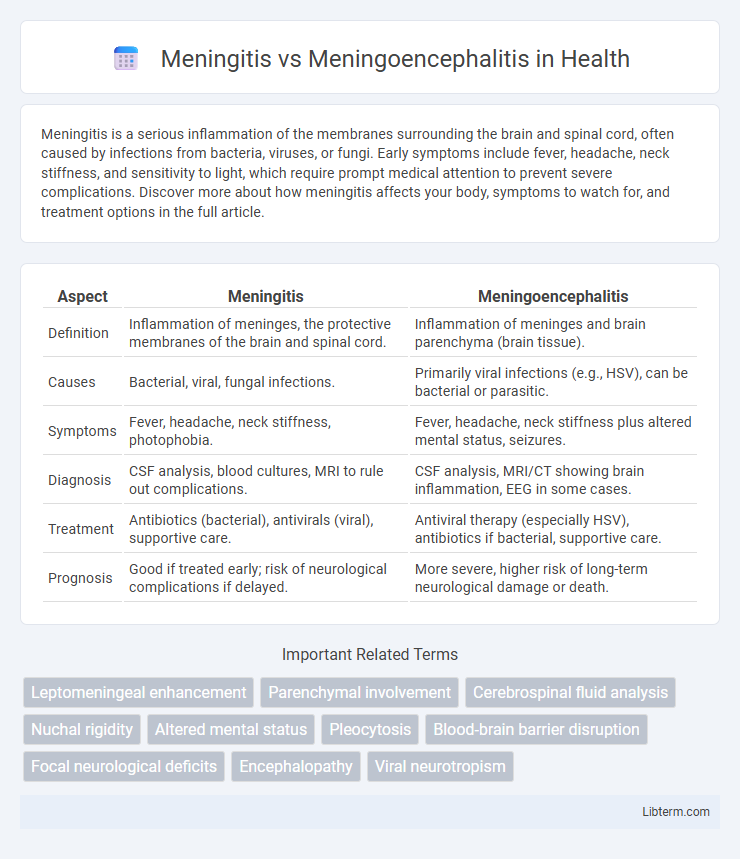
| Aspect | Meningitis | Meningoencephalitis |
|---|---|---|
| Definition | Inflammation of meninges, the protective membranes of the brain and spinal cord. | Inflammation of meninges and brain parenchyma (brain tissue). |
| Causes | Bacterial, viral, fungal infections. | Primarily viral infections (e.g., HSV), can be bacterial or parasitic. |
| Symptoms | Fever, headache, neck stiffness, photophobia. | Fever, headache, neck stiffness plus altered mental status, seizures. |
| Diagnosis | CSF analysis, blood cultures, MRI to rule out complications. | CSF analysis, MRI/CT showing brain inflammation, EEG in some cases. |
| Treatment | Antibiotics (bacterial), antivirals (viral), supportive care. | Antiviral therapy (especially HSV), antibiotics if bacterial, supportive care. |
| Prognosis | Good if treated early; risk of neurological complications if delayed. | More severe, higher risk of long-term neurological damage or death. |
Understanding Meningitis: Definition and Causes
Meningitis is the inflammation of the protective membranes covering the brain and spinal cord, known as the meninges, caused by bacterial, viral, or fungal infections. Common bacterial pathogens include Neisseria meningitidis and Streptococcus pneumoniae, while viral meningitis often results from enteroviruses. In contrast, meningoencephalitis involves inflammation of both the meninges and the brain tissue, typically caused by viral infections such as herpes simplex virus.
What is Meningoencephalitis? Key Differences
Meningoencephalitis is an inflammation that affects both the meninges, the protective membranes surrounding the brain and spinal cord, and the brain tissue itself, often caused by viral or bacterial infections. Unlike meningitis, which involves only the meninges, meningoencephalitis presents with more severe neurological symptoms such as altered mental status, seizures, and focal neurological deficits. Early diagnosis and treatment are critical to prevent complications like brain damage or death, highlighting the importance of distinguishing meningoencephalitis from meningitis in clinical practice.
Etiology: Common Pathogens and Risk Factors
Meningitis primarily results from infections by Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae, with viruses such as enteroviruses also contributing to viral meningitis; risk factors include age extremes, immunosuppression, and close living conditions. Meningoencephalitis, involving inflammation of both the meninges and brain tissue, is commonly caused by herpes simplex virus (HSV-1), arboviruses like West Nile virus, and occasionally bacterial agents; immunocompromised states and exposure to vectors increase susceptibility. Differentiating these conditions hinges on pathogen identification and patient history, which guide targeted antimicrobial or antiviral therapy.
Clinical Presentation: Signs and Symptoms Comparison
Meningitis primarily presents with sudden onset of fever, headache, neck stiffness, and photophobia, often accompanied by nausea and vomiting. Meningoencephalitis shares these symptoms but typically includes altered mental status, seizures, and focal neurological deficits due to brain parenchyma involvement. Differentiating signs such as behavioral changes and decreased consciousness in meningoencephalitis are critical for diagnosis and management.
Diagnostic Approaches: Tests and Imaging
Meningitis diagnosis primarily involves cerebrospinal fluid (CSF) analysis through lumbar puncture, assessing white blood cell count, glucose, and protein levels, alongside bacterial cultures or PCR for pathogen identification. Meningoencephalitis diagnosis incorporates similar CSF testing but often requires brain imaging such as MRI to detect inflammation or damage in brain tissue. Electroencephalography (EEG) is also useful in meningoencephalitis cases to evaluate encephalopathic changes and seizure activity.
Cerebrospinal Fluid Findings: Distinguishing Features
Cerebrospinal fluid (CSF) analysis in meningitis typically reveals elevated white blood cell counts with a predominance of neutrophils, increased protein levels, and low glucose concentration, indicating bacterial infection. In meningoencephalitis, CSF findings may show a mixed cellular response with both lymphocytes and neutrophils, moderately elevated protein, and normal or slightly decreased glucose, reflecting viral or atypical infectious involvement of both meninges and brain parenchyma. Distinguishing these patterns in CSF profiles aids in differentiating pure meningeal inflammation from combined meningeal and encephalitic processes, guiding targeted therapeutic interventions.
Treatment Strategies: Antibiotics, Antivirals, and Supportive Care
Treatment strategies for meningitis primarily involve targeted antibiotic therapy for bacterial cases and antiviral medications for viral infections, while meningoencephalitis requires a combination of antibiotics or antivirals depending on the causative pathogen alongside aggressive supportive care to manage neurological complications. Early administration of broad-spectrum antibiotics like ceftriaxone or ampicillin is critical for bacterial meningitis, whereas antiviral agents such as acyclovir are essential for herpes simplex virus-induced meningoencephalitis. Supportive care includes intracranial pressure management, seizure control, hydration, and respiratory support to optimize patient outcomes and reduce the risk of long-term neurological impairments.
Prognosis and Potential Complications
Meningitis primarily affects the protective membranes of the brain and spinal cord, often resulting in symptoms like severe headache, fever, and neck stiffness, with a prognosis largely dependent on early diagnosis and treatment, typically favorable in bacterial cases if promptly managed. Meningoencephalitis involves simultaneous inflammation of both the meninges and brain tissue, leading to more severe neurological impairments such as seizures, cognitive deficits, and higher mortality rates, especially in viral or autoimmune etiologies. Potential complications of meningitis include hearing loss, brain damage, and hydrocephalus, whereas meningoencephalitis patients face increased risks of long-term neurological disabilities, persistent brain inflammation, and increased intracranial pressure.
Prevention Measures: Vaccination and Prophylaxis
Vaccination remains the most effective prevention measure against meningitis, targeting key pathogens such as Neisseria meningitidis, Streptococcus pneumoniae, and Haemophilus influenzae type b. Prophylactic antibiotics play a critical role in preventing meningococcal disease transmission among close contacts of affected individuals. Maintaining up-to-date immunization schedules and implementing chemoprophylaxis protocols significantly reduce the incidence of both meningitis and meningoencephalitis.
Meningitis vs Meningoencephalitis: Key Takeaways and Summary
Meningitis primarily involves inflammation of the protective membranes covering the brain and spinal cord, often caused by bacterial, viral, or fungal infections. Meningoencephalitis presents as a more severe condition combining meningitis with encephalitis, resulting in inflammation of both the meninges and brain tissue, frequently leading to neurological complications. Timely diagnosis and treatment are crucial for both, with meningoencephalitis requiring more intensive management due to its broader impact on the central nervous system.
Meningitis Infographic
 libterm.com
libterm.com