Neovascularization refers to the process of new blood vessel formation, crucial for tissue repair and regeneration in response to injury or ischemia. This physiological phenomenon plays a vital role in healing wounds, restoring blood flow, and supporting organ function. Explore the full article to understand how neovascularization impacts your health and potential therapeutic approaches.
Table of Comparison
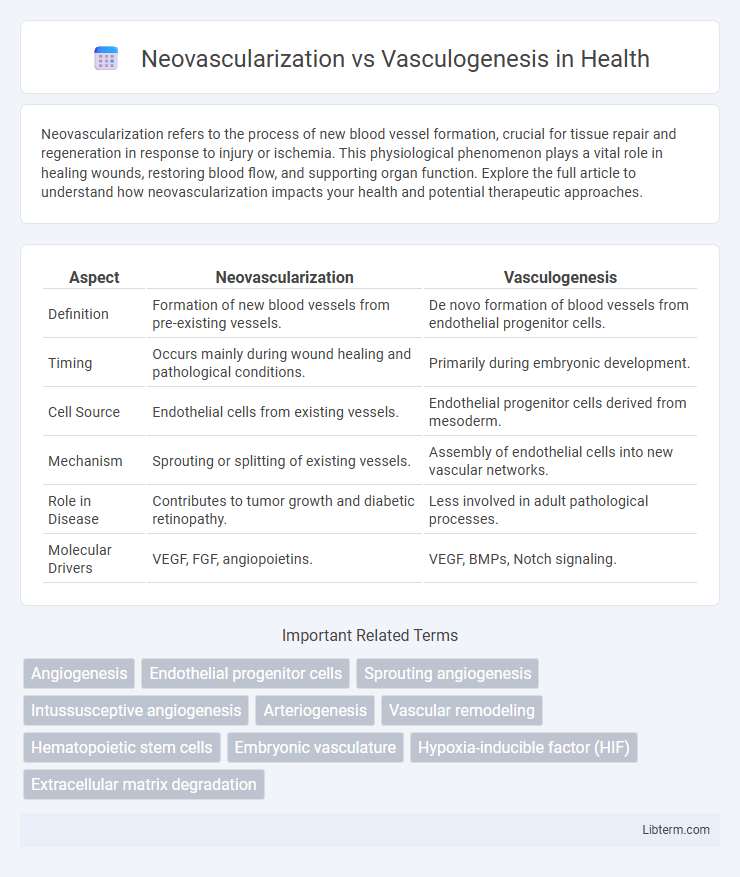
| Aspect | Neovascularization | Vasculogenesis |
|---|---|---|
| Definition | Formation of new blood vessels from pre-existing vessels. | De novo formation of blood vessels from endothelial progenitor cells. |
| Timing | Occurs mainly during wound healing and pathological conditions. | Primarily during embryonic development. |
| Cell Source | Endothelial cells from existing vessels. | Endothelial progenitor cells derived from mesoderm. |
| Mechanism | Sprouting or splitting of existing vessels. | Assembly of endothelial cells into new vascular networks. |
| Role in Disease | Contributes to tumor growth and diabetic retinopathy. | Less involved in adult pathological processes. |
| Molecular Drivers | VEGF, FGF, angiopoietins. | VEGF, BMPs, Notch signaling. |
Introduction to Neovascularization and Vasculogenesis
Neovascularization refers to the formation of new blood vessels from pre-existing vasculature, primarily through angiogenesis and arteriogenesis, critical in tissue repair and pathological conditions like cancer. Vasculogenesis involves the de novo assembly of endothelial cells into primitive vascular networks, predominantly occurring during embryonic development but also contributing to adult neovascular processes. Both mechanisms are essential for establishing and remodeling the vascular system, with distinct cellular origins and molecular pathways driving their unique roles.
Defining Neovascularization: Process and Significance
Neovascularization is the physiological process through which new blood vessels form from pre-existing vasculature, playing a crucial role in wound healing, tissue regeneration, and tumor growth. This process involves endothelial cell proliferation, migration, and organization into new capillary networks, facilitating oxygen and nutrient delivery to ischemic or damaged tissues. Unlike vasculogenesis, which occurs during embryonic development through the differentiation of angioblasts into endothelial cells, neovascularization primarily occurs postnatally and is vital for adapting vascular supply to changing tissue demands.
Understanding Vasculogenesis: Origins and Mechanisms
Vasculogenesis is the process through which new blood vessels form de novo from endothelial progenitor cells during embryonic development, distinct from neovascularization that mainly involves vessel sprouting from pre-existing vasculature. This mechanism originates in mesoderm-derived angioblasts that differentiate and assemble into primitive vascular networks, establishing the primary circulatory framework. Key molecular signals such as vascular endothelial growth factor (VEGF) and angiopoietins regulate endothelial cell migration, proliferation, and tube formation in vasculogenesis.
Key Differences Between Neovascularization and Vasculogenesis
Neovascularization involves the formation of new blood vessels from pre-existing vessels, primarily through angiogenesis and arteriogenesis, whereas vasculogenesis is the de novo formation of blood vessels from endothelial progenitor cells during embryonic development or tissue repair. Neovascularization plays a crucial role in wound healing and tumor growth by remodeling existing vascular networks, while vasculogenesis establishes initial vascular networks in early embryogenesis and contributes to vascular regeneration in adults. The key distinction lies in neovascularization relying on existing vascular structures, whereas vasculogenesis originates from endothelial precursor cells without pre-existing vessels.
Molecular Pathways Involved in Neovascularization
Neovascularization primarily involves the activation of molecular pathways such as VEGF (vascular endothelial growth factor), Notch signaling, and angiopoietins, which regulate endothelial cell proliferation, migration, and differentiation. The VEGF pathway triggers hypoxia-inducible factors (HIFs), promoting angiogenesis by stimulating existing blood vessels to sprout new capillaries. Notch signaling modulates vessel maturation and branching, while angiopoietins maintain vessel stability and permeability during the neovascularization process.
Cellular Mechanisms of Vasculogenesis
Vasculogenesis involves the differentiation of endothelial progenitor cells into mature endothelial cells, forming new blood vessels primarily during embryonic development. This process is driven by key signaling pathways such as VEGF (vascular endothelial growth factor) and the Notch pathway, which regulate cell migration, proliferation, and organization. Unlike neovascularization, which relies on the remodeling and sprouting of existing vessels, vasculogenesis generates vascular structures de novo from progenitor cells.
Physiological and Pathological Contexts
Neovascularization involves the formation of new blood vessels from existing ones, playing a critical role in wound healing and tissue repair, while vasculogenesis refers to the de novo formation of blood vessels from endothelial progenitor cells primarily during embryonic development. In pathological contexts, neovascularization contributes to tumor growth and diabetic retinopathy by promoting abnormal vessel proliferation, whereas vasculogenesis is implicated in tissue regeneration and ischemic disease recovery through mobilization of bone marrow-derived endothelial progenitors. Both processes are essential for maintaining vascular homeostasis but differ fundamentally in their cellular origins and roles in health and disease.
Clinical Implications in Disease and Therapy
Neovascularization primarily refers to the formation of new blood vessels from existing vasculature, playing a crucial role in wound healing, tumor growth, and ischemic diseases. Vasculogenesis, the de novo formation of blood vessels from endothelial progenitor cells, is critical during embryonic development and is increasingly recognized for therapeutic angiogenesis in cardiovascular diseases. Understanding the distinct mechanisms of neovascularization and vasculogenesis informs targeted therapies, such as anti-angiogenic drugs for cancer and pro-angiogenic strategies in regenerative medicine.
Advances in Research and Therapeutic Angiogenesis
Recent advances in neovascularization research emphasize the role of endothelial cell sprouting and remodeling during new blood vessel formation, contrasting with vasculogenesis, which involves de novo differentiation of endothelial progenitor cells from mesodermal precursors. Therapeutic angiogenesis exploits growth factors such as VEGF and FGF to stimulate neovascularization in ischemic tissues, advancing treatments for cardiovascular diseases and tissue regeneration. Cutting-edge techniques, including gene therapy and biomaterial scaffolds, enhance targeted delivery and efficacy, marking significant progress in clinical applications of angiogenesis modulation.
Future Perspectives and Emerging Trends
Emerging trends in neovascularization versus vasculogenesis emphasize advanced biomaterial scaffolds and gene editing technologies like CRISPR to enhance therapeutic angiogenesis in tissue engineering and regenerative medicine. Future perspectives highlight integration of single-cell sequencing and artificial intelligence to unravel cellular heterogeneity and streamline personalized vascular repair strategies. Innovations in endothelial progenitor cell mobilization and extracellular vesicle-based therapies are poised to revolutionize clinical applications targeting ischemic diseases and wound healing.
Neovascularization Infographic
 libterm.com
libterm.com