Gout and osteoarthritis are common forms of arthritis that affect joint health, with gout caused by uric acid crystal buildup and osteoarthritis resulting from cartilage degeneration. Both conditions can cause severe pain and stiffness, impacting your daily activities and overall quality of life. Discover how to manage symptoms and improve joint function by reading the rest of this article.
Table of Comparison
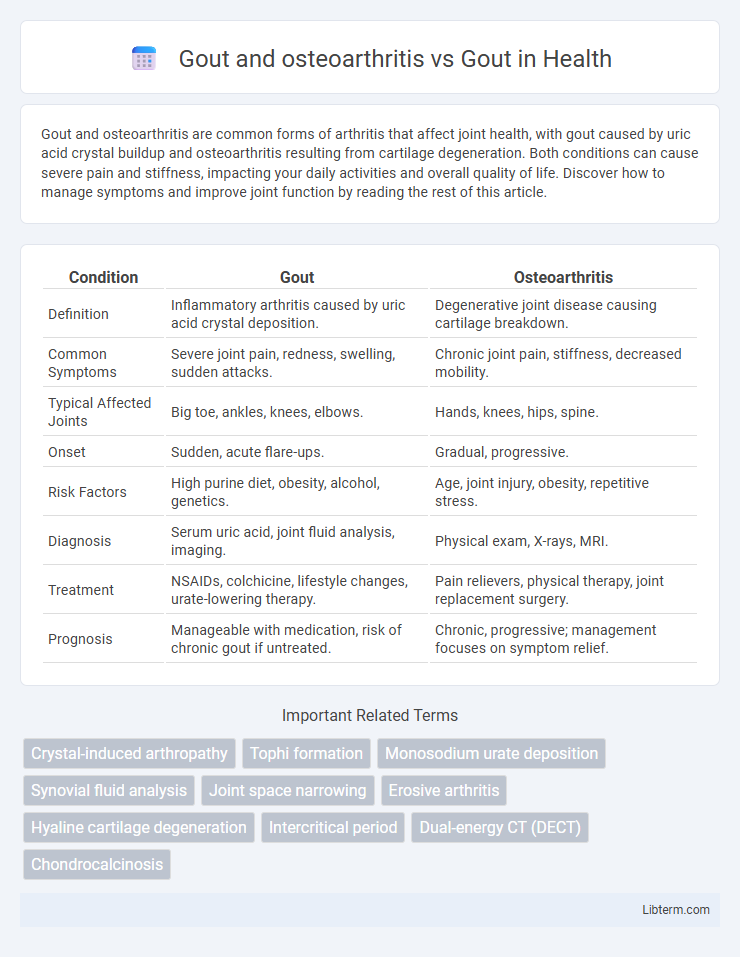
| Condition | Gout | Osteoarthritis |
|---|---|---|
| Definition | Inflammatory arthritis caused by uric acid crystal deposition. | Degenerative joint disease causing cartilage breakdown. |
| Common Symptoms | Severe joint pain, redness, swelling, sudden attacks. | Chronic joint pain, stiffness, decreased mobility. |
| Typical Affected Joints | Big toe, ankles, knees, elbows. | Hands, knees, hips, spine. |
| Onset | Sudden, acute flare-ups. | Gradual, progressive. |
| Risk Factors | High purine diet, obesity, alcohol, genetics. | Age, joint injury, obesity, repetitive stress. |
| Diagnosis | Serum uric acid, joint fluid analysis, imaging. | Physical exam, X-rays, MRI. |
| Treatment | NSAIDs, colchicine, lifestyle changes, urate-lowering therapy. | Pain relievers, physical therapy, joint replacement surgery. |
| Prognosis | Manageable with medication, risk of chronic gout if untreated. | Chronic, progressive; management focuses on symptom relief. |
Understanding Gout: Causes and Symptoms
Gout is a type of inflammatory arthritis caused by the accumulation of monosodium urate crystals due to hyperuricemia, leading to sudden and severe joint pain, redness, and swelling, often affecting the big toe. Osteoarthritis, in contrast, involves the gradual degeneration of cartilage and joint tissues, presenting with chronic pain and stiffness primarily in weight-bearing joints. Understanding gout's causes, including dietary factors, genetics, and kidney function, is essential for differentiating it from osteoarthritis and initiating appropriate treatment to prevent recurrent flare-ups and joint damage.
Defining Osteoarthritis: Key Differences from Gout
Osteoarthritis is a degenerative joint disease characterized by the breakdown of cartilage and bone changes, primarily affecting weight-bearing joints such as knees and hips. Unlike gout, which is caused by urate crystal deposition leading to acute inflammation, osteoarthritis involves gradual joint wear and tear without crystal buildup. Key differences include osteoarthritis's chronic progression and cartilage deterioration versus gout's episodic flares and inflammatory response to uric acid crystals.
Overlapping Features: Gout vs. Osteoarthritis
Gout and osteoarthritis share overlapping features such as joint pain, swelling, and stiffness primarily affecting the lower limbs, especially the big toe and knees. Both conditions involve inflammation and cartilage damage, but gout is characterized by urate crystal deposition while osteoarthritis results from cartilage degeneration and bone remodeling. Differentiating these disorders relies on identifying acute gout flares with elevated serum uric acid and tophi, contrasting with the chronic, progressive joint space narrowing seen in osteoarthritis.
Joint Damage: How Gout and Osteoarthritis Affect Mobility
Gout causes sudden, intense joint inflammation primarily due to urate crystal buildup, leading to severe pain and swelling that temporarily impairs mobility. Osteoarthritis gradually deteriorates cartilage, causing chronic joint stiffness and reduced range of motion, significantly affecting long-term mobility. When gout coexists with osteoarthritis, joint damage accelerates, exacerbating pain and further restricting movement.
Diagnostic Criteria: Differentiating Gout and Osteoarthritis
Diagnostic criteria for gout emphasize the identification of monosodium urate crystals in synovial fluid or a tophus, alongside acute onset of intense joint pain, erythema, and swelling, typically in the first metatarsophalangeal joint. Osteoarthritis diagnosis relies on radiographic evidence of joint space narrowing, osteophyte formation, and subchondral sclerosis, with chronic joint pain and stiffness predominant in weight-bearing joints like the knees and hips. Differentiating gout from osteoarthritis hinges on laboratory analysis of synovial fluid and clinical presentation, where gout manifests as episodic inflammatory arthritis, while osteoarthritis presents as a progressive degenerative joint disease.
Risk Factors for Gout and Osteoarthritis
Gout primarily arises from hyperuricemia, which leads to the deposition of monosodium urate crystals in joints, with risk factors including obesity, excessive alcohol consumption, high purine diet, and genetic predisposition. Osteoarthritis risk factors focus on joint wear and tear caused by aging, obesity, joint injury, and repetitive mechanical stress. Both conditions share obesity as a significant risk factor, but gout is uniquely influenced by metabolic and dietary factors, whereas osteoarthritis is mainly associated with biomechanical and age-related joint degeneration.
Pain Management: Comparing Treatment Approaches
Pain management in gout primarily involves acute anti-inflammatory medications like NSAIDs, colchicine, and corticosteroids to reduce intense joint inflammation and pain during flare-ups, while osteoarthritis treatment focuses on long-term alleviation through analgesics, physical therapy, and lifestyle modifications. Gout pain is episodic and intensely sharp due to urate crystal deposition, whereas osteoarthritis pain is chronic, arising from cartilage degeneration and joint wear. Combining urate-lowering therapy with targeted pain relief is essential in gout, whereas addressing mechanical joint stress and inflammation is central to osteoarthritis management.
Lifestyle Modifications for Gout and Osteoarthritis Patients
Effective lifestyle modifications for gout and osteoarthritis patients emphasize weight management, a balanced diet low in purines, and regular low-impact exercise to reduce joint pain and inflammation. Staying hydrated and avoiding alcohol and sugary beverages help lower uric acid levels in gout, while physical therapy and strengthening exercises improve joint function and mobility in osteoarthritis. These combined approaches support symptom relief and enhance overall quality of life for individuals managing both conditions.
Long-Term Complications: What to Expect
Gout often leads to chronic joint inflammation and the formation of tophi, which can cause joint damage over time, while osteoarthritis primarily results in cartilage degradation and bone spurs that worsen joint function. Long-term complications of gout include recurrent acute attacks, joint deformities, and increased risk of kidney stones due to high uric acid levels. Both conditions may cause chronic pain and reduced mobility, but gout's systemic effects also pose unique risks such as cardiovascular disease and renal impairment.
Preventive Strategies: Reducing the Risk of Joint Disease
Preventive strategies for gout and osteoarthritis involve targeted lifestyle modifications and medical management to reduce uric acid levels and joint wear. Maintaining a balanced diet low in purines, regular exercise, and weight control are effective in minimizing gout flare-ups and osteoarthritis progression. Pharmacologic interventions such as allopurinol for gout and NSAIDs for osteoarthritis complement these approaches by controlling inflammation and preserving joint function.
Gout and osteoarthritis Infographic
 libterm.com
libterm.com