Hypermagnesemia occurs when magnesium levels in the blood exceed normal limits, leading to symptoms such as muscle weakness, fatigue, and irregular heartbeat. This condition often results from kidney dysfunction, excessive magnesium intake, or certain medications affecting magnesium balance. Learn more about the causes, symptoms, and treatments of hypermagnesemia in the rest of this article.
Table of Comparison
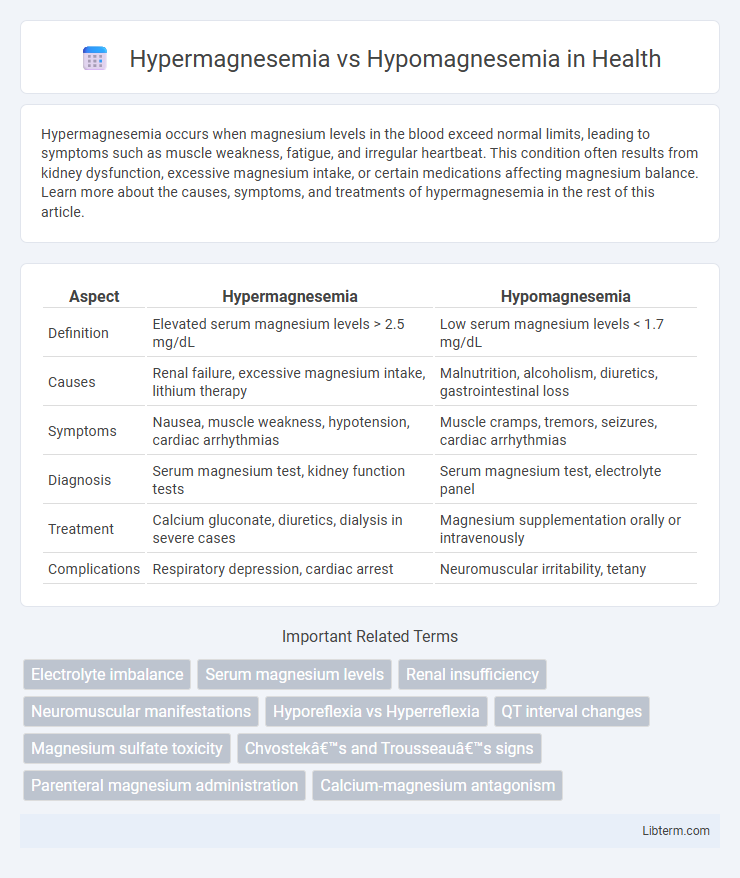
| Aspect | Hypermagnesemia | Hypomagnesemia |
|---|---|---|
| Definition | Elevated serum magnesium levels > 2.5 mg/dL | Low serum magnesium levels < 1.7 mg/dL |
| Causes | Renal failure, excessive magnesium intake, lithium therapy | Malnutrition, alcoholism, diuretics, gastrointestinal loss |
| Symptoms | Nausea, muscle weakness, hypotension, cardiac arrhythmias | Muscle cramps, tremors, seizures, cardiac arrhythmias |
| Diagnosis | Serum magnesium test, kidney function tests | Serum magnesium test, electrolyte panel |
| Treatment | Calcium gluconate, diuretics, dialysis in severe cases | Magnesium supplementation orally or intravenously |
| Complications | Respiratory depression, cardiac arrest | Neuromuscular irritability, tetany |
Introduction to Magnesium Homeostasis
Magnesium homeostasis is critical for maintaining physiological functions, with the kidneys playing a central role in regulating serum magnesium levels through filtration and reabsorption. Hypermagnesemia occurs when magnesium concentrations exceed the normal reference range of 1.7 to 2.2 mg/dL, often due to impaired renal excretion or excessive intake. Conversely, hypomagnesemia is characterized by serum magnesium levels below 1.7 mg/dL, commonly resulting from inadequate absorption, increased renal loss, or gastrointestinal disorders that disrupt magnesium balance.
Definition: Hypermagnesemia vs Hypomagnesemia
Hypermagnesemia is a condition characterized by abnormally high levels of magnesium in the blood, typically exceeding 2.5 mg/dL, often caused by kidney failure or excessive magnesium intake. Hypomagnesemia refers to low serum magnesium levels below 1.7 mg/dL, frequently resulting from malnutrition, chronic diarrhea, or certain medications such as diuretics. Both disorders disrupt neuromuscular and cardiovascular function but differ fundamentally in their magnesium concentration and underlying etiologies.
Causes of Hypermagnesemia
Hypermagnesemia primarily results from excessive magnesium intake through supplements or medications, especially in patients with chronic kidney disease where renal excretion is impaired. Other causes include adrenal insufficiency, hypothyroidism, and the use of magnesium-containing antacids or laxatives. In contrast, hypomagnesemia commonly arises from gastrointestinal losses, malnutrition, chronic alcoholism, or certain diuretics that increase magnesium excretion.
Causes of Hypomagnesemia
Hypomagnesemia primarily results from gastrointestinal losses due to chronic diarrhea, malabsorption syndromes, or prolonged proton pump inhibitor use, leading to decreased magnesium absorption. Renal losses are also significant, often caused by diuretics, alcohol abuse, or genetic tubular disorders that impair magnesium reabsorption. Other causes include inadequate dietary intake, especially in malnourished or chronic alcoholics, resulting in critically low serum magnesium levels essential for neuromuscular and cardiac function.
Signs and Symptoms Comparison
Hypermagnesemia presents with signs such as muscle weakness, hypotension, and respiratory depression, often accompanied by lethargy and nausea. In contrast, hypomagnesemia symptoms include neuromuscular irritability, tremors, tetany, and cardiac arrhythmias like torsades de pointes. Both conditions impact magnesium levels critically, influencing muscle function and cardiovascular stability.
Diagnostic Criteria and Laboratory Findings
Hypermagnesemia is diagnosed when serum magnesium levels exceed 2.5 mg/dL, often associated with renal failure or excessive magnesium intake, characterized by symptoms such as hypotension and muscle weakness; laboratory findings reveal elevated serum magnesium along with potential hyperkalemia and hypercalcemia. Hypomagnesemia is defined by serum magnesium levels below 1.7 mg/dL, commonly linked to malnutrition, alcoholism, or gastrointestinal losses, presenting with neuromuscular irritability and arrhythmias; laboratory tests show low serum magnesium, frequently accompanied by hypokalemia and hypocalcemia. Accurate diagnosis requires measuring serum magnesium concentration alongside electrolyte panels to identify underlying imbalances critical for treatment management.
Pathophysiological Mechanisms
Hypermagnesemia results from impaired renal magnesium excretion or excessive magnesium intake, leading to inhibited calcium channels and neuromuscular depression, while hypomagnesemia arises from poor dietary intake, gastrointestinal losses, or renal wasting, causing increased cellular excitability due to dysregulated ion transport. The pathophysiology of hypermagnesemia involves decreased release of acetylcholine at neuromuscular junctions and cardiac conduction abnormalities, whereas hypomagnesemia disrupts potassium and calcium homeostasis, enhancing neuromuscular irritability and arrhythmogenic potential. Both conditions impact magnesium's role as a critical cofactor in enzymatic reactions and ion channel regulation, influencing cellular signaling and electrophysiological stability.
Treatment Strategies for Hypermagnesemia
Treatment strategies for hypermagnesemia primarily involve discontinuing magnesium-containing medications and administration of intravenous calcium gluconate to antagonize the effects of elevated magnesium on cardiac and neuromuscular function. Enhanced renal excretion through diuretics like furosemide combined with aggressive intravenous hydration helps reduce serum magnesium levels in patients with adequate kidney function. In severe cases, especially with renal failure, hemodialysis is the most effective intervention to rapidly lower magnesium concentrations.
Treatment Strategies for Hypomagnesemia
Treatment strategies for hypomagnesemia focus on magnesium replacement through oral supplements such as magnesium oxide or magnesium chloride for mild cases, while severe hypomagnesemia requires intravenous magnesium sulfate administration. Monitoring serum magnesium levels and correcting underlying causes like gastrointestinal losses or diuretic use is essential for effective management. Maintaining adequate magnesium intake through diet or supplementation helps prevent recurrence and supports overall electrolyte balance.
Prevention and Clinical Management Tips
Maintaining serum magnesium levels between 1.7 and 2.2 mg/dL is crucial to prevent hypermagnesemia and hypomagnesemia, which can be achieved by monitoring dietary intake and adjusting supplements accordingly. Clinical management of hypermagnesemia involves discontinuing magnesium-containing drugs and administering calcium gluconate to antagonize magnesium's cardiac effects, along with diuretics or dialysis for severe cases. Hypomagnesemia treatment focuses on oral or intravenous magnesium replacement, addressing underlying causes such as malabsorption or diuretic use, and regular monitoring of electrolytes to avoid recurrent deficiency.
Hypermagnesemia Infographic
 libterm.com
libterm.com