Acute pancreatitis is a sudden inflammation of the pancreas that can cause severe abdominal pain and digestive issues. Early diagnosis and appropriate treatment are crucial to prevent complications and support recovery. Explore the rest of the article to learn how to recognize symptoms and manage this condition effectively.
Table of Comparison
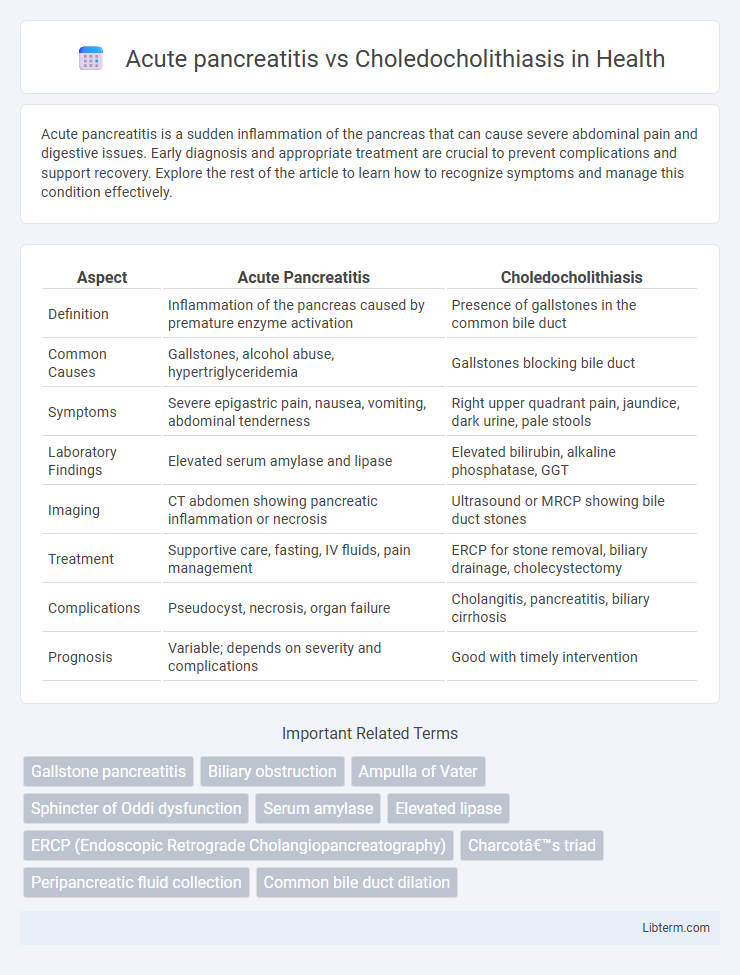
| Aspect | Acute Pancreatitis | Choledocholithiasis |
|---|---|---|
| Definition | Inflammation of the pancreas caused by premature enzyme activation | Presence of gallstones in the common bile duct |
| Common Causes | Gallstones, alcohol abuse, hypertriglyceridemia | Gallstones blocking bile duct |
| Symptoms | Severe epigastric pain, nausea, vomiting, abdominal tenderness | Right upper quadrant pain, jaundice, dark urine, pale stools |
| Laboratory Findings | Elevated serum amylase and lipase | Elevated bilirubin, alkaline phosphatase, GGT |
| Imaging | CT abdomen showing pancreatic inflammation or necrosis | Ultrasound or MRCP showing bile duct stones |
| Treatment | Supportive care, fasting, IV fluids, pain management | ERCP for stone removal, biliary drainage, cholecystectomy |
| Complications | Pseudocyst, necrosis, organ failure | Cholangitis, pancreatitis, biliary cirrhosis |
| Prognosis | Variable; depends on severity and complications | Good with timely intervention |
Introduction to Acute Pancreatitis and Choledocholithiasis
Acute pancreatitis is an inflammatory condition of the pancreas characterized by sudden onset of abdominal pain and elevated pancreatic enzymes, often triggered by gallstones or alcohol use. Choledocholithiasis involves the presence of gallstones in the common bile duct, leading to bile flow obstruction and potential complications such as jaundice, cholangitis, or pancreatitis. Both conditions share overlapping clinical features but require distinct diagnostic and therapeutic approaches to address their respective pathophysiologies.
Definition and Overview of Acute Pancreatitis
Acute pancreatitis is a sudden inflammation of the pancreas characterized by severe abdominal pain and elevated pancreatic enzymes, often caused by gallstones or alcohol abuse. Choledocholithiasis refers to the presence of gallstones in the common bile duct, which can obstruct bile flow and lead to complications like pancreatitis. Differentiating acute pancreatitis from choledocholithiasis is crucial for targeted treatment, as pancreatitis primarily involves pancreatic inflammation, while choledocholithiasis centers on biliary obstruction.
Definition and Overview of Choledocholithiasis
Choledocholithiasis refers to the presence of one or more gallstones in the common bile duct, often leading to bile flow obstruction and potential complications such as jaundice and cholangitis. Acute pancreatitis is an inflammatory condition of the pancreas frequently caused by gallstones blocking the pancreatic duct, with choledocholithiasis being a common underlying etiology. Understanding choledocholithiasis involves recognizing its role in biliary obstruction, its impact on pancreatic function, and its diagnostic evaluation through imaging techniques like ERCP or MRCP.
Etiology and Risk Factors
Acute pancreatitis commonly results from gallstones obstructing the pancreatic duct or from chronic alcohol use, with gallstone-induced pancreatitis accounting for approximately 40-70% of cases. Choledocholithiasis, characterized by the presence of stones in the common bile duct, primarily arises from gallstone migration and is associated with risk factors including age over 40, female sex, obesity, and a history of gallbladder disease. Both conditions share gallstones as a central etiology, but choledocholithiasis specifically implicates bile duct obstruction leading to cholestasis and possible secondary infections.
Pathophysiology: Mechanisms of Disease
Acute pancreatitis results from premature activation of pancreatic enzymes causing autodigestion and inflammation, often triggered by gallstones or alcohol. Choledocholithiasis involves obstruction of the common bile duct by gallstones, leading to bile duct inflammation and impaired bile flow. Both conditions share pathophysiological features related to biliary obstruction, but pancreatitis centers on pancreatic enzyme activation, while choledocholithiasis primarily involves cholestasis and biliary inflammation.
Clinical Presentation and Symptoms
Acute pancreatitis typically presents with sudden, severe epigastric pain radiating to the back, accompanied by nausea and vomiting, while choledocholithiasis often causes intermittent right upper quadrant pain, jaundice, and dark urine due to biliary obstruction. Elevated serum amylase and lipase levels are hallmark indicators in acute pancreatitis, whereas cholestatic liver enzyme patterns with elevated alkaline phosphatase and bilirubin suggest choledocholithiasis. Both conditions may involve abdominal tenderness, but the presence of fever and signs of infection more commonly point toward choledocholithiasis with ascending cholangitis.
Diagnostic Approaches and Imaging
Diagnostic approaches for acute pancreatitis primarily include serum amylase and lipase measurement, with lipase being more specific, while choledocholithiasis diagnosis relies on liver function tests indicating cholestasis. Imaging techniques for acute pancreatitis start with abdominal ultrasound to exclude gallstones and can progress to contrast-enhanced CT scan for assessing severity and complications. Magnetic resonance cholangiopancreatography (MRCP) and endoscopic ultrasound (EUS) offer high sensitivity in detecting choledocholithiasis, providing detailed visualization of bile duct stones without ionizing radiation.
Laboratory Findings and Biomarkers
Acute pancreatitis typically presents with elevated serum amylase and lipase levels, with lipase being more specific and remaining elevated longer. In choledocholithiasis, liver function tests such as alkaline phosphatase, gamma-glutamyl transferase (GGT), and bilirubin are predominantly elevated due to bile duct obstruction. Elevated C-reactive protein (CRP) can be found in both conditions, reflecting inflammation, but pancreatic enzymes are primarily diagnostic for acute pancreatitis, whereas cholestatic liver enzymes indicate choledocholithiasis.
Treatment Strategies and Management Options
Acute pancreatitis treatment primarily involves supportive care such as fluid resuscitation, pain control, and nutritional support, with severe cases requiring intensive monitoring and possible intervention for complications. Choledocholithiasis management focuses on relieving biliary obstruction through endoscopic retrograde cholangiopancreatography (ERCP) with stone extraction, followed by cholecystectomy to prevent recurrence. Both conditions necessitate addressing underlying causes and monitoring for complications like infection or organ failure to optimize patient outcomes.
Prognosis, Complications, and Prevention
Acute pancreatitis presents a variable prognosis dependent on severity, with mild cases resolving quickly, while severe forms can lead to systemic inflammatory response syndrome and multi-organ failure. Choledocholithiasis often necessitates endoscopic removal to prevent complications like cholangitis, biliary cirrhosis, or pancreatitis, with prognosis improving significantly post-intervention. Prevention for acute pancreatitis emphasizes managing risk factors such as gallstones and alcohol use, whereas choledocholithiasis prevention includes dietary regulation, maintaining bile flow, and addressing underlying gallstone disease.
Acute pancreatitis Infographic
 libterm.com
libterm.com