Conscious sedation is a medically controlled state that helps you stay relaxed and comfortable during minor procedures without losing full consciousness. This technique balances pain relief and anxiety reduction while allowing you to respond to commands and breathe independently. Explore the rest of the article to understand how conscious sedation can enhance your procedure experience safely and effectively.
Table of Comparison
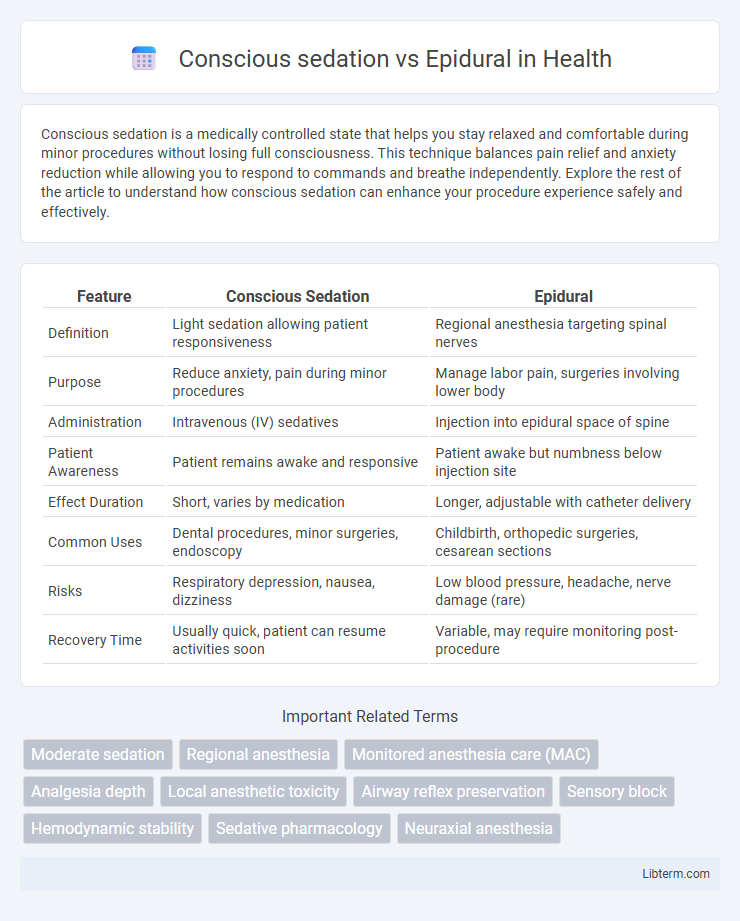
| Feature | Conscious Sedation | Epidural |
|---|---|---|
| Definition | Light sedation allowing patient responsiveness | Regional anesthesia targeting spinal nerves |
| Purpose | Reduce anxiety, pain during minor procedures | Manage labor pain, surgeries involving lower body |
| Administration | Intravenous (IV) sedatives | Injection into epidural space of spine |
| Patient Awareness | Patient remains awake and responsive | Patient awake but numbness below injection site |
| Effect Duration | Short, varies by medication | Longer, adjustable with catheter delivery |
| Common Uses | Dental procedures, minor surgeries, endoscopy | Childbirth, orthopedic surgeries, cesarean sections |
| Risks | Respiratory depression, nausea, dizziness | Low blood pressure, headache, nerve damage (rare) |
| Recovery Time | Usually quick, patient can resume activities soon | Variable, may require monitoring post-procedure |
Introduction to Conscious Sedation and Epidural
Conscious sedation is a medically controlled state of depressed consciousness that allows patients to remain awake and responsive while reducing pain and anxiety during procedures. An epidural involves the injection of anesthetic near the spinal nerves to block pain from a specific region, commonly used during labor or lower body surgeries. Both methods provide effective pain management but differ in administration, depth of sedation, and recovery times.
Definition and Mechanism of Conscious Sedation
Conscious sedation is a minimally invasive technique that uses sedative medications to relax patients while maintaining their ability to respond to verbal commands, often employed during minor surgical or diagnostic procedures. Its mechanism involves the administration of drugs like benzodiazepines or opioids that depress the central nervous system to induce a state of calm and partial amnesia without full loss of consciousness. In contrast, an epidural is a regional anesthesia method delivering local anesthetics near the spinal nerves to block pain sensation in specific body areas, typically used during labor or major surgeries.
Overview and Process of Epidural Anesthesia
Epidural anesthesia involves the injection of a local anesthetic into the epidural space surrounding the spinal cord, numbing the lower body while allowing the patient to remain awake and alert. The procedure typically begins with the patient sitting or lying on their side, followed by the insertion of a needle and catheter into the epidural space, through which medication is administered to block nerve impulses. Unlike conscious sedation, which induces a relaxed and minimally sedated state without full pain blockade, epidural anesthesia provides targeted and profound pain relief primarily used during labor, surgeries, or chronic pain management.
Indications: When to Use Conscious Sedation vs Epidural
Conscious sedation is indicated for minor surgical procedures, dental treatments, or endoscopic exams requiring patient relaxation without complete loss of consciousness, allowing for quick recovery and cooperation. Epidural anesthesia is primarily used in labor and delivery, major lower body surgeries, and chronic pain management to provide targeted and effective pain relief with minimal systemic sedation. Choice depends on the procedure's invasiveness, patient health status, and desired pain control level, with epidurals preferred for extensive and prolonged pain management.
Procedure and Administration Techniques
Conscious sedation involves administering sedative medications intravenously to induce relaxation while maintaining patient responsiveness, typically monitored through continuous vital signs and oxygen saturation. Epidural anesthesia requires the insertion of a catheter into the epidural space of the spinal column, delivering local anesthetics that block nerve signals in targeted regions, often guided by anatomical landmarks or fluoroscopy. Both techniques necessitate trained professionals for precise dosing and placement to ensure patient safety and effective pain management during procedures.
Efficacy and Pain Control Comparison
Conscious sedation provides moderate pain relief by depressing the central nervous system while maintaining patient responsiveness, making it effective for minor procedures with minimal discomfort. Epidural anesthesia offers superior pain control by blocking nerve impulses in the targeted area, proving highly effective for labor and major surgeries with prolonged pain relief. Studies demonstrate epidurals achieve better analgesia and patient satisfaction compared to conscious sedation during invasive or extended procedures.
Safety Profile and Common Side Effects
Conscious sedation provides moderate sedation allowing patients to remain responsive, with common side effects including nausea, dizziness, and mild respiratory depression, while maintaining a strong safety profile under proper monitoring. Epidural anesthesia offers targeted numbness, frequently used during labor or surgery, carrying risks of hypotension, headache, and rare nerve damage but generally considered safe with vigilant technique. Both methods require careful patient assessment to minimize complications, prioritizing individualized approaches for maximum safety and efficacy.
Patient Eligibility and Contraindications
Conscious sedation is suitable for patients requiring minor procedures who are able to maintain airway reflexes and follow instructions, but it is contraindicated in individuals with severe respiratory disorders or allergies to sedative agents. Epidural anesthesia is ideal for patients undergoing labor or lower limb surgeries, especially when general anesthesia poses higher risks; however, it is contraindicated in patients with coagulopathy, infection at the injection site, or severe hypovolemia. Careful assessment of medical history, coagulation status, and airway management capabilities is critical to determine the appropriate anesthesia modality and ensure patient safety.
Recovery Time and Post-Procedure Considerations
Conscious sedation typically allows for a quicker recovery time, with patients often regaining full alertness within 30 to 60 minutes post-procedure, whereas epidural anesthesia may result in longer recovery due to residual numbness and potential motor blockade lasting several hours. Post-procedure considerations for conscious sedation include monitoring for respiratory depression and ensuring patient orientation, while epidural care involves assessing sensory and motor function return, managing potential complications like hypotension or urinary retention. Choosing between conscious sedation and epidural anesthesia hinges on procedure type, patient health status, and recovery priorities, with conscious sedation preferred for shorter, less invasive procedures and epidurals favored for pain control during labor or major lower body surgeries.
Making the Right Choice: Factors for Decision Making
Choosing between conscious sedation and epidural anesthesia depends on factors such as the procedure type, patient medical history, and pain management preferences. Conscious sedation offers relaxation and partial awareness suitable for minor surgeries, while epidural provides targeted pain relief ideal for childbirth or lower body procedures. Evaluation of risks, recovery time, and potential side effects guides clinicians in tailoring anesthesia choices to individual patient needs for optimal outcomes.
Conscious sedation Infographic
 libterm.com
libterm.com