An outbreak occurs when a sudden increase in the number of cases of a disease happens within a specific population or area, rapidly spreading and posing significant health risks. Effective outbreak management involves early detection, swift response, and community engagement to control transmission and protect vulnerable groups. Discover how your awareness and timely action can make a difference by exploring the rest of this article.
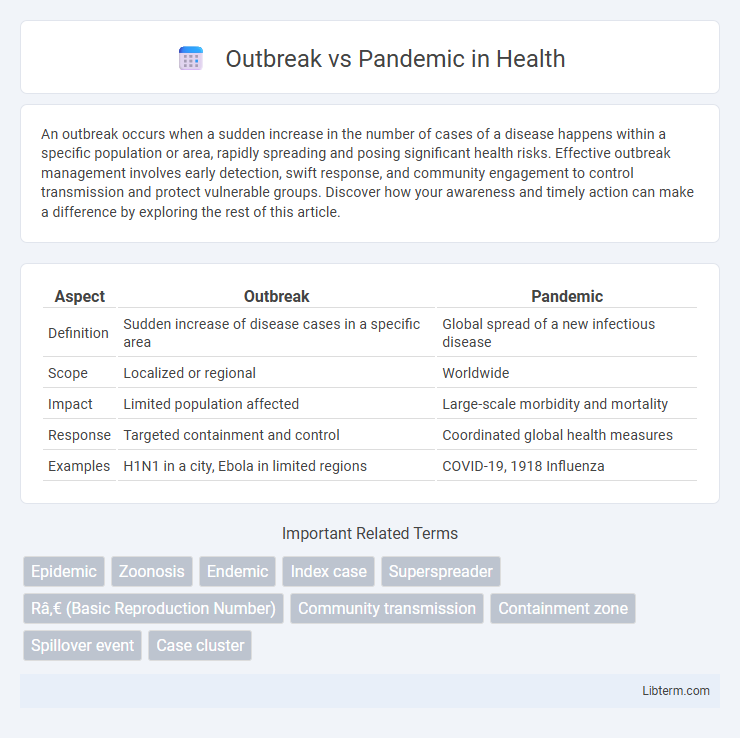
Table of Comparison
| Aspect | Outbreak | Pandemic |
|---|---|---|
| Definition | Sudden increase of disease cases in a specific area | Global spread of a new infectious disease |
| Scope | Localized or regional | Worldwide |
| Impact | Limited population affected | Large-scale morbidity and mortality |
| Response | Targeted containment and control | Coordinated global health measures |
| Examples | H1N1 in a city, Ebola in limited regions | COVID-19, 1918 Influenza |
Understanding Outbreaks: Definition and Scope
An outbreak refers to the sudden occurrence of a disease in a specific place and time, affecting a limited and localized population. It involves a rapid increase in cases beyond what is normally expected, often confined to a community, region, or institution. Understanding outbreaks requires analyzing transmission dynamics, identifying the source, and implementing containment measures to prevent escalation into larger epidemics or pandemics.
What Constitutes a Pandemic?
A pandemic is characterized by the widespread and sustained transmission of an infectious disease across multiple countries or continents, affecting a large portion of the global population. Unlike an outbreak, which is typically localized to a specific community or region, a pandemic demonstrates high levels of contagion and global spread, often overwhelming healthcare systems worldwide. The World Health Organization (WHO) defines a pandemic based on factors including geographic spread, disease severity, and the impact on society and healthcare infrastructure.
Key Differences Between Outbreaks and Pandemics
Outbreaks refer to the sudden occurrence of a disease in a specific geographic area or population, often limited in scope and duration. Pandemics represent a global spread of a disease affecting multiple countries or continents with sustained community transmission and high infection rates. Key differences include scale, with outbreaks being localized and pandemics widespread, and impact severity, where pandemics generally cause significant health, social, and economic consequences worldwide.
Causes and Triggers of Infectious Disease Spread
Outbreaks occur when a specific infectious disease rapidly infects a localized population due to factors like environmental changes, human behavior, or introduction of a pathogen. Pandemics emerge when an outbreak escalates globally, driven by high transmission rates, viral mutations, and increased human mobility such as international travel. Key triggers include zoonotic spillover events, inadequate public health infrastructure, and delayed containment measures.
Stages of Disease Escalation: From Outbreak to Pandemic
An outbreak represents a sudden increase in cases of a disease within a localized area, indicating the initial stage of disease escalation. When the infection spreads beyond borders, affecting multiple countries or continents with sustained community transmission, it transitions into an epidemic and subsequently a pandemic. Understanding these stages is vital for implementing appropriate public health responses and containment measures.
Global Impact: Outbreaks vs. Pandemics
Outbreaks are localized surges of infectious diseases affecting specific communities or regions, often containing limited global impact. In contrast, pandemics involve widespread disease transmission across multiple countries or continents, causing significant disruption to global health systems, economies, and societies. The extensive reach of pandemics necessitates coordinated international responses to mitigate their far-reaching consequences.
Response Strategies for Outbreaks and Pandemics
Response strategies for outbreaks prioritize rapid containment measures such as targeted quarantines, localized testing, and immediate contact tracing to prevent further spread. Pandemic responses require coordinated international efforts, widespread vaccination campaigns, large-scale healthcare resource allocation, and continuous public communication to manage extensive transmission across countries. Effective management hinges on early detection systems and adaptive policies tailored to the scale and severity of the infectious event.
Historical Examples: Major Outbreaks vs. Famous Pandemics
The 1918 influenza outbreak, often called the Spanish Flu pandemic, resulted in millions of deaths worldwide, distinguishing it as one of the deadliest pandemics in history. In contrast, the 2003 SARS outbreak was more localized, affecting primarily East Asia with fewer cases but rapid containment. The COVID-19 pandemic, emerging in late 2019, demonstrated global spread and long-term impact unlike localized outbreaks such as the 2014 Ebola outbreak confined mainly to West Africa.
The Role of Public Health Organizations
Public health organizations play a critical role in containing outbreaks by implementing rapid response measures such as contact tracing, vaccination campaigns, and localized quarantine protocols. During a pandemic, these organizations coordinate international efforts to monitor virus spread, allocate healthcare resources, and develop public communication strategies to mitigate global impact. Effective collaboration between entities like the World Health Organization (WHO), Centers for Disease Control and Prevention (CDC), and local health departments is essential to transition from outbreak containment to pandemic management.
Prevention and Preparedness for Future Threats
Effective prevention of outbreaks and pandemics relies on robust surveillance systems and rapid response mechanisms to detect and contain infectious diseases early. Strengthening healthcare infrastructure, promoting widespread vaccination, and enhancing public health education are critical for improving preparedness against future threats. Collaborative international efforts and investment in research for novel therapeutics and vaccines ensure resilience and minimize the impact of global health emergencies.
Outbreak Infographic
 libterm.com
libterm.com