Hypokalemia is a medical condition characterized by low potassium levels in the blood, which can lead to muscle weakness, cramps, and irregular heart rhythms. Proper diagnosis and treatment are essential to prevent severe complications and maintain heart and muscle function. Discover how you can recognize symptoms, causes, and effective treatments by reading the rest of this article.
Table of Comparison
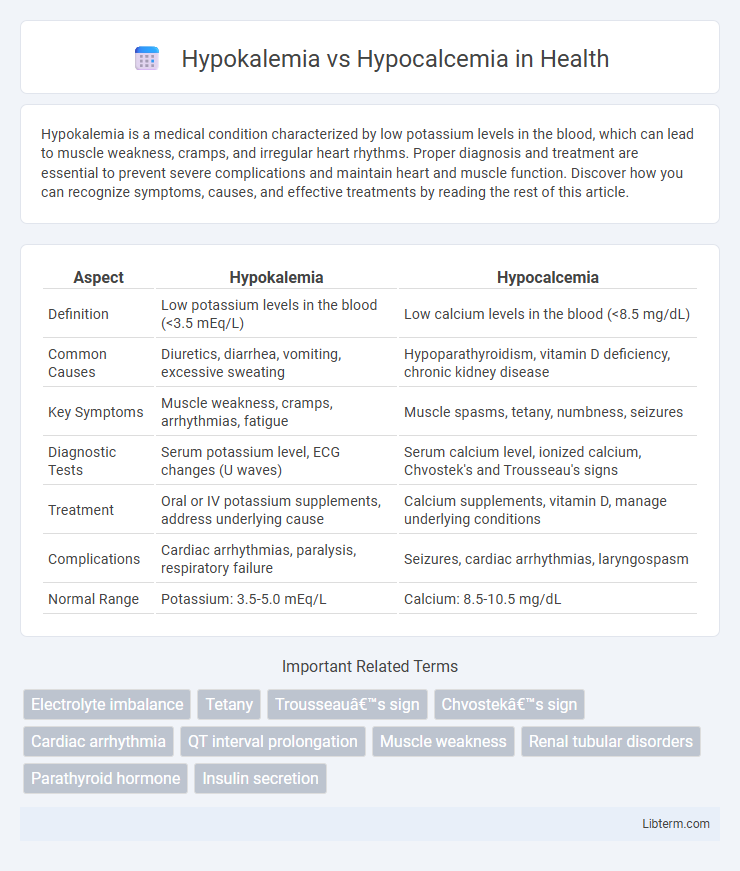
| Aspect | Hypokalemia | Hypocalcemia |
|---|---|---|
| Definition | Low potassium levels in the blood (<3.5 mEq/L) | Low calcium levels in the blood (<8.5 mg/dL) |
| Common Causes | Diuretics, diarrhea, vomiting, excessive sweating | Hypoparathyroidism, vitamin D deficiency, chronic kidney disease |
| Key Symptoms | Muscle weakness, cramps, arrhythmias, fatigue | Muscle spasms, tetany, numbness, seizures |
| Diagnostic Tests | Serum potassium level, ECG changes (U waves) | Serum calcium level, ionized calcium, Chvostek's and Trousseau's signs |
| Treatment | Oral or IV potassium supplements, address underlying cause | Calcium supplements, vitamin D, manage underlying conditions |
| Complications | Cardiac arrhythmias, paralysis, respiratory failure | Seizures, cardiac arrhythmias, laryngospasm |
| Normal Range | Potassium: 3.5-5.0 mEq/L | Calcium: 8.5-10.5 mg/dL |
Overview of Hypokalemia and Hypocalcemia
Hypokalemia is characterized by low potassium levels in the blood, often below 3.5 mEq/L, leading to symptoms such as muscle weakness, cramps, and cardiac arrhythmias. Hypocalcemia involves decreased serum calcium levels, typically under 8.5 mg/dL, resulting in neuromuscular irritability, tetany, and potential cardiac complications. Both electrolyte imbalances require prompt diagnosis and management to prevent severe physiological disruptions.
Key Differences in Electrolyte Balance
Hypokalemia refers to low potassium levels in the blood, typically below 3.5 mEq/L, disrupting cellular functions such as muscle contraction and nerve transmission. Hypocalcemia involves reduced calcium concentration, generally less than 8.5 mg/dL, affecting bone strength and neuromuscular excitability. The key difference lies in their specific electrolyte imbalances: potassium influences cardiac and muscular electrical activity, while calcium primarily regulates bone metabolism and neuromuscular signaling.
Causes and Risk Factors
Hypokalemia primarily results from excessive potassium loss due to diuretics, vomiting, or diarrhea, with risk factors including chronic kidney disease and certain endocrine disorders such as hyperaldosteronism. Hypocalcemia often arises from vitamin D deficiency, hypoparathyroidism, or chronic kidney failure, with risk factors including malabsorption syndromes and post-thyroidectomy states. Both electrolyte imbalances require attention to underlying causes for effective management and prevention.
Clinical Manifestations
Hypokalemia presents with muscle weakness, cramps, fatigue, and cardiac arrhythmias due to decreased potassium levels in the blood. Hypocalcemia manifests as neuromuscular irritability, including tetany, muscle spasms, numbness, and positive Chvostek's and Trousseau's signs, resulting from low calcium concentration. Both conditions can cause cardiac abnormalities, but hypocalcemia more commonly leads to prolonged QT interval, whereas hypokalemia often results in U waves on electrocardiogram.
Diagnostic Approaches
Diagnostic approaches for hypokalemia involve measuring serum potassium levels below 3.5 mEq/L, assessing urinary potassium excretion to differentiate renal from extrarenal losses, and conducting electrocardiograms to identify characteristic arrhythmias or U waves. For hypocalcemia, serum calcium measurement is essential, including total and ionized calcium levels, along with albumin correction; supplementary tests like parathyroid hormone (PTH) levels, vitamin D status, and magnesium concentrations help determine underlying causes. Advanced diagnostics may include imaging studies such as neck ultrasound or sestamibi scans for hypocalcemia when hypoparathyroidism or parathyroid adenoma is suspected.
Laboratory Findings Comparison
Hypokalemia presents with low serum potassium levels typically below 3.5 mEq/L, often accompanied by metabolic alkalosis and U-wave changes on ECG. Hypocalcemia is characterized by serum calcium levels under 8.5 mg/dL, with laboratory findings showing decreased ionized calcium and prolonged QT interval on ECG. Both conditions require electrolyte panels, but hypokalemia specifically alters potassium ion concentration while hypocalcemia impacts total and ionized calcium levels.
Treatment and Management Strategies
Hypokalemia treatment typically involves oral or intravenous potassium replacement, with close monitoring of cardiac function to prevent arrhythmias, whereas hypocalcemia management centers on calcium supplementation, either orally or intravenously, often accompanied by vitamin D to enhance calcium absorption. Both conditions require addressing underlying causes such as renal loss, gastrointestinal issues, or medication effects to prevent recurrence. Regular serum electrolyte monitoring and symptom assessment are critical for effective management and avoiding complications like muscle weakness in hypokalemia or tetany and seizures in hypocalcemia.
Potential Complications
Hypokalemia can cause life-threatening cardiac arrhythmias, muscle weakness, and respiratory failure due to impaired neuromuscular function. Hypocalcemia often leads to tetany, seizures, and prolonged QT interval, increasing the risk of ventricular arrhythmias and heart failure. Both electrolyte imbalances require prompt recognition and correction to prevent severe neuromuscular and cardiovascular complications.
Prevention and Monitoring
Preventing hypokalemia involves ensuring adequate dietary potassium intake through foods like bananas, oranges, and spinach, while avoiding excessive use of diuretics or laxatives that deplete potassium levels. Hypocalcemia prevention requires maintaining sufficient calcium and vitamin D intake, monitoring parathyroid function, and managing conditions such as chronic kidney disease or malabsorption syndromes. Regular monitoring of serum potassium and calcium levels through blood tests aids early detection and guides timely intervention to avoid complications associated with these electrolyte imbalances.
Prognosis and Long-term Outcomes
Hypokalemia prognosis depends on the severity and underlying cause, with mild cases often resolving without long-term effects, while severe or untreated hypokalemia can lead to cardiac arrhythmias and muscle weakness, increasing morbidity risk. Hypocalcemia prognosis varies based on etiology; chronic hypocalcemia may result in neurological complications, such as seizures and cognitive impairment, and long-term management often requires calcium and vitamin D supplementation to prevent bone demineralization. Both conditions necessitate monitoring electrolyte levels to prevent complications and improve patient outcomes through targeted therapy.
Hypokalemia Infographic
 libterm.com
libterm.com