Single morbidity refers to the presence of one chronic illness or health condition in an individual, impacting their daily life and healthcare needs. Managing this condition effectively requires understanding symptoms, treatment options, and lifestyle adjustments tailored to your specific health status. Explore the rest of the article to learn strategies for coping with single morbidity and improving your well-being.
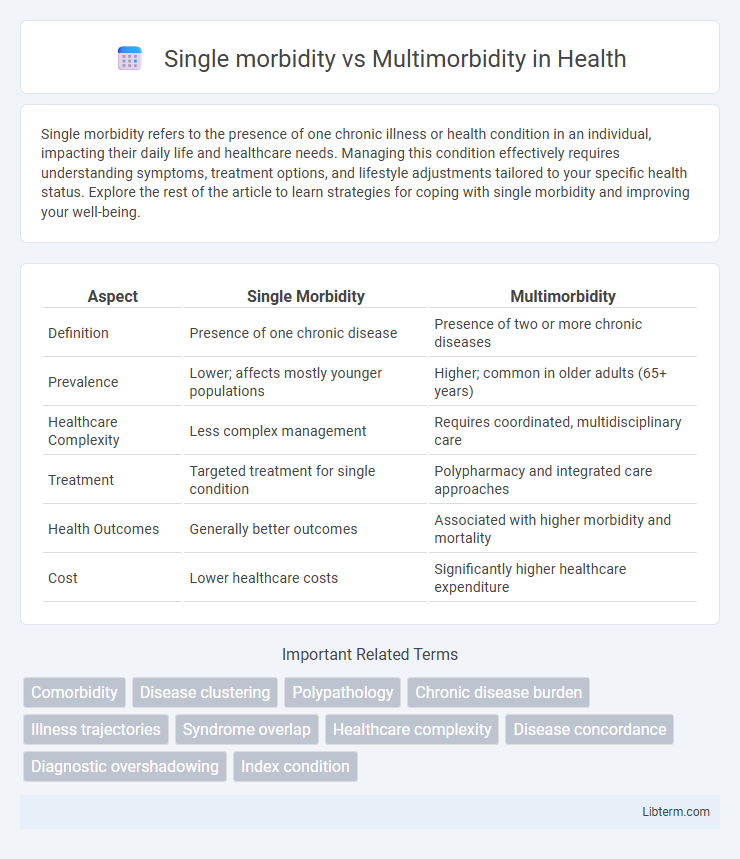
Table of Comparison
| Aspect | Single Morbidity | Multimorbidity |
|---|---|---|
| Definition | Presence of one chronic disease | Presence of two or more chronic diseases |
| Prevalence | Lower; affects mostly younger populations | Higher; common in older adults (65+ years) |
| Healthcare Complexity | Less complex management | Requires coordinated, multidisciplinary care |
| Treatment | Targeted treatment for single condition | Polypharmacy and integrated care approaches |
| Health Outcomes | Generally better outcomes | Associated with higher morbidity and mortality |
| Cost | Lower healthcare costs | Significantly higher healthcare expenditure |
Defining Single Morbidity
Single morbidity refers to the presence of one distinct chronic disease or medical condition in an individual, such as diabetes or hypertension. This condition requires targeted management and treatment plans specific to that single illness. Effective care for single morbidity emphasizes disease-specific interventions to improve patient outcomes and quality of life.
Understanding Multimorbidity
Multimorbidity refers to the coexistence of two or more chronic conditions in an individual, significantly impacting treatment complexity and healthcare outcomes compared to single morbidity cases. Understanding multimorbidity involves recognizing the interactions between diseases, such as diabetes, hypertension, and heart disease, which can exacerbate symptoms and complicate medication management. Comprehensive care models and personalized treatment plans are essential to address the multifactorial needs and improve quality of life for patients with multimorbidity.
Epidemiology of Single Morbidity
Single morbidity refers to the presence of one chronic disease in an individual, with epidemiological studies showing varying prevalence rates depending on the disease type and population demographics. Common single morbid conditions include hypertension, diabetes mellitus, and chronic respiratory diseases, which significantly contribute to global disease burden and healthcare resource utilization. Epidemiological data emphasize age, lifestyle factors, and socio-economic status as key determinants influencing the incidence and prevalence of single morbidity worldwide.
Prevalence and Patterns of Multimorbidity
Multimorbidity, characterized by the co-occurrence of two or more chronic conditions, affects approximately 25-30% of the adult population globally, with higher prevalence seen in elderly and socioeconomically disadvantaged groups. Patterns of multimorbidity often include clusters of cardiovascular diseases, diabetes, osteoarthritis, and depression, revealing common pathophysiological pathways and risk factors. Understanding these multimorbidity patterns is critical for developing targeted healthcare interventions and resource allocation to improve patient outcomes and reduce healthcare costs.
Risk Factors for Single Morbidity
Single morbidity refers to the presence of one chronic disease in an individual, often influenced by risk factors such as genetic predisposition, lifestyle behaviors like smoking, poor diet, physical inactivity, and environmental exposures. Key determinants include age, socioeconomic status, and access to healthcare, which significantly affect disease onset and progression. Understanding these risk factors is critical for targeted prevention and management strategies to reduce the burden of single chronic conditions.
Causes and Contributing Factors of Multimorbidity
Multimorbidity arises from a complex interplay of genetic predisposition, aging, and lifestyle factors such as poor nutrition, physical inactivity, and chronic stress. Environmental exposures including pollution and socioeconomic determinants like limited access to healthcare or education also significantly contribute to the development of multiple chronic conditions. Chronic inflammation and comorbid mental health disorders further exacerbate the risk, differentiating multimorbidity from single morbidity that typically involves isolated disease causes.
Clinical Management: Single vs. Multiple Conditions
Clinical management of single morbidity typically involves targeted treatment protocols addressing one disease, allowing for streamlined medication regimens and focused monitoring. In contrast, multimorbidity requires integrated care plans that manage multiple conditions simultaneously, emphasizing coordination among specialists to optimize treatment and avoid adverse drug interactions. Effective management of multimorbidity also necessitates personalized approaches that consider patient complexity, polypharmacy risks, and the potential for overlapping symptoms and complications.
Healthcare Challenges in Multimorbidity
Multimorbidity, the coexistence of two or more chronic conditions, poses significant healthcare challenges compared to single morbidity due to its complexity and the need for integrated care plans. Patients with multimorbidity experience higher rates of hospitalizations, polypharmacy, and fragmented care, increasing the risk of adverse drug interactions and medical errors. Healthcare systems struggle to provide coordinated, patient-centered services that address multiple conditions simultaneously, highlighting the necessity for multidisciplinary approaches and enhanced communication among providers.
Impact on Patient Quality of Life
Single morbidity typically affects patient quality of life by limiting daily activities and increasing dependence on healthcare resources, but the impact is often more predictable and manageable. Multimorbidity significantly reduces quality of life due to the complex interplay of multiple chronic conditions, leading to increased symptom burden, polypharmacy risks, and higher healthcare utilization. Patients with multimorbidity experience more severe physical and psychological distress, resulting in greater functional impairment and diminished well-being compared to those with a single morbidity.
Strategies for Prevention and Intervention
Effective prevention strategies for single morbidity primarily emphasize targeted lifestyle modifications and early screening for specific diseases such as diabetes or hypertension. In contrast, multimorbidity requires integrated care models that address multiple chronic conditions simultaneously, utilizing comprehensive medication management and coordinated primary care interventions. Both approaches benefit from patient education, but multimorbidity prevention increasingly relies on multidisciplinary teams and personalized care plans to manage complex health needs.
Single morbidity Infographic
 libterm.com
libterm.com