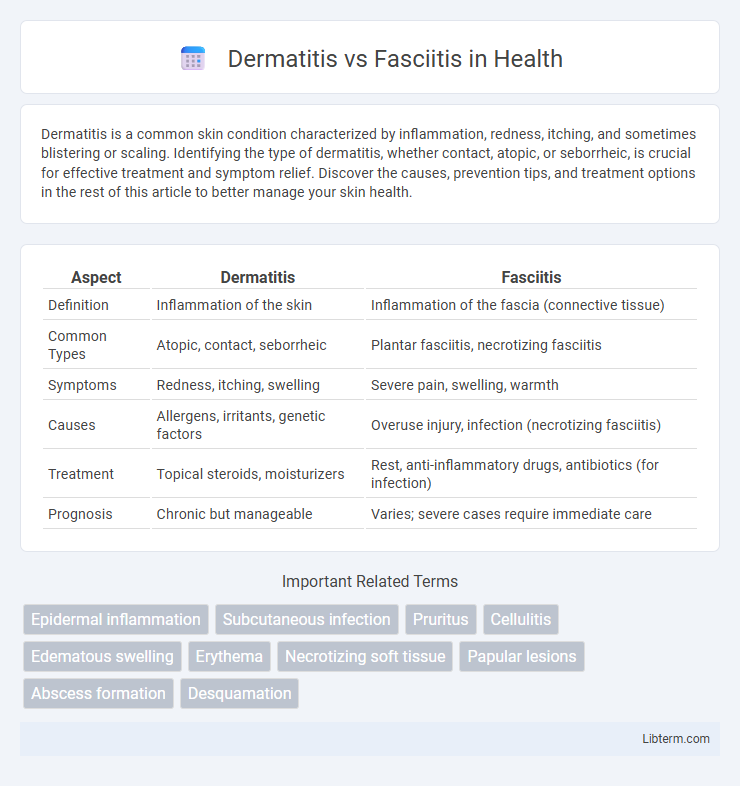
Dermatitis is a common skin condition characterized by inflammation, redness, itching, and sometimes blistering or scaling. Identifying the type of dermatitis, whether contact, atopic, or seborrheic, is crucial for effective treatment and symptom relief. Discover the causes, prevention tips, and treatment options in the rest of this article to better manage your skin health.
Table of Comparison
| Aspect | Dermatitis | Fasciitis |
|---|---|---|
| Definition | Inflammation of the skin | Inflammation of the fascia (connective tissue) |
| Common Types | Atopic, contact, seborrheic | Plantar fasciitis, necrotizing fasciitis |
| Symptoms | Redness, itching, swelling | Severe pain, swelling, warmth |
| Causes | Allergens, irritants, genetic factors | Overuse injury, infection (necrotizing fasciitis) |
| Treatment | Topical steroids, moisturizers | Rest, anti-inflammatory drugs, antibiotics (for infection) |
| Prognosis | Chronic but manageable | Varies; severe cases require immediate care |
Understanding Dermatitis: Definition and Causes
Dermatitis is an inflammatory skin condition characterized by redness, itching, and swelling, caused by various factors such as allergens, irritants, and genetic predisposition. Common types include atopic dermatitis, contact dermatitis, and seborrheic dermatitis, each with specific triggers like chemicals, environmental factors, or immune responses. Understanding the underlying causes helps in effective management and prevention, differentiating it from fasciitis, which primarily affects the fascia and involves deeper tissue inflammation.
What is Fasciitis? Key Characteristics
Fasciitis is an inflammation of the fascia, a thick connective tissue layer surrounding muscles, nerves, and blood vessels, commonly resulting in severe pain and swelling. The most notable type, plantar fasciitis, affects the foot's fascia causing heel pain, stiffness, and difficulty walking. Key characteristics include localized tenderness, especially in the heel or arch area, along with increased pain during movement or after periods of rest.
Symptoms: Dermatitis vs Fasciitis
Dermatitis symptoms primarily include itchy, red, and inflamed skin, often accompanied by dryness, scaling, and sometimes blistering or oozing. Fasciitis manifests with deep, severe pain, swelling, tenderness, and warmth over the affected fascia, often limiting movement due to underlying tissue inflammation. Unlike dermatitis, fasciitis typically involves more intense pain and underlying connective tissue damage rather than superficial skin irritation.
Common Types of Dermatitis
Common types of dermatitis include atopic dermatitis, contact dermatitis, and seborrheic dermatitis, each characterized by inflammation, itching, and redness of the skin. Fasciitis, in contrast, involves inflammation of the fascia, the connective tissue surrounding muscles, and is commonly associated with conditions such as plantar fasciitis or necrotizing fasciitis, which affect deeper tissues rather than the skin surface. Understanding these distinctions aids in accurate diagnosis and targeted treatment for skin-related versus connective tissue inflammatory conditions.
Varieties of Fasciitis Explained
Fasciitis encompasses several varieties, including plantar fasciitis, which affects the thick band of tissue on the bottom of the foot, and necrotizing fasciitis, a severe bacterial infection causing rapid tissue death. Another type, eosinophilic fasciitis, involves inflammation and thickening of the skin and fascia, often linked to autoimmune responses. These varieties differ significantly from dermatitis, which primarily affects the skin's surface and involves inflammation, redness, and itching without the deeper tissue damage seen in fasciitis.
Risk Factors and Triggers
Dermatitis risk factors include genetic predisposition, exposure to irritants such as soaps and chemicals, and allergens like pollen or pet dander, while triggers often involve dry skin, stress, and environmental changes. Fasciitis, particularly plantar fasciitis, is commonly associated with risk factors like obesity, prolonged standing, improper footwear, and foot structure abnormalities, with triggers including repetitive strain, sudden increases in physical activity, and inadequate stretching. Both conditions may worsen with lifestyle factors but require distinct management approaches due to differing pathophysiologies.
Diagnosis: Distinguishing Between Dermatitis and Fasciitis
Accurate diagnosis between dermatitis and fasciitis relies on clinical examination and diagnostic imaging. Dermatitis presents with erythema, scaling, and itching, often localized to the skin surface, whereas fasciitis typically manifests as deep tissue pain, swelling, and limited mobility, reflecting inflammation of the fascia. Biopsy and MRI are key diagnostic tools, with biopsy confirming skin pathology in dermatitis and MRI revealing fascial thickening or inflammation in fasciitis.
Treatment Approaches for Dermatitis
Topical corticosteroids remain the primary treatment approach for dermatitis, effectively reducing inflammation and itching. Emollients and moisturizers are essential in restoring skin barrier function and preventing dryness, while antihistamines can help control severe itching. In cases of infection or severe inflammation, systemic corticosteroids or antibiotics may be prescribed to manage symptoms and promote healing.
Management and Treatment of Fasciitis
Management of fasciitis primarily involves prompt administration of antibiotics to address bacterial infections, especially in cases of necrotizing fasciitis, alongside surgical debridement to remove necrotic tissue and prevent further spread. Supportive care including pain control, fluid resuscitation, and wound care is critical for optimal recovery. Early diagnosis and aggressive intervention are essential to reduce morbidity and improve patient outcomes in fasciitis treatment.
Prevention and When to Seek Medical Help
Preventing dermatitis involves maintaining good skin hygiene, avoiding irritants and allergens, and using moisturizers to keep the skin barrier intact, while fasciitis prevention focuses on proper footwear, regular stretching, and avoiding repetitive strain on the fascia, especially in plantar fasciitis cases. Seek medical help for dermatitis if symptoms worsen, such as increased redness, swelling, or signs of infection like pus, and for fasciitis when pain persists beyond a few weeks, limits mobility, or causes severe discomfort despite home treatments. Early diagnosis and treatment can prevent complications and promote faster recovery for both conditions.
Dermatitis Infographic
 libterm.com
libterm.com