Acute tubular necrosis is a kidney disorder characterized by the death of tubular epithelial cells, often caused by ischemia or nephrotoxic agents, leading to acute kidney injury and impaired renal function. Early diagnosis and treatment focus on identifying the underlying cause and managing symptoms to prevent permanent kidney damage. Explore the rest of the article to understand how you can recognize symptoms, treatment options, and recovery processes.
Table of Comparison
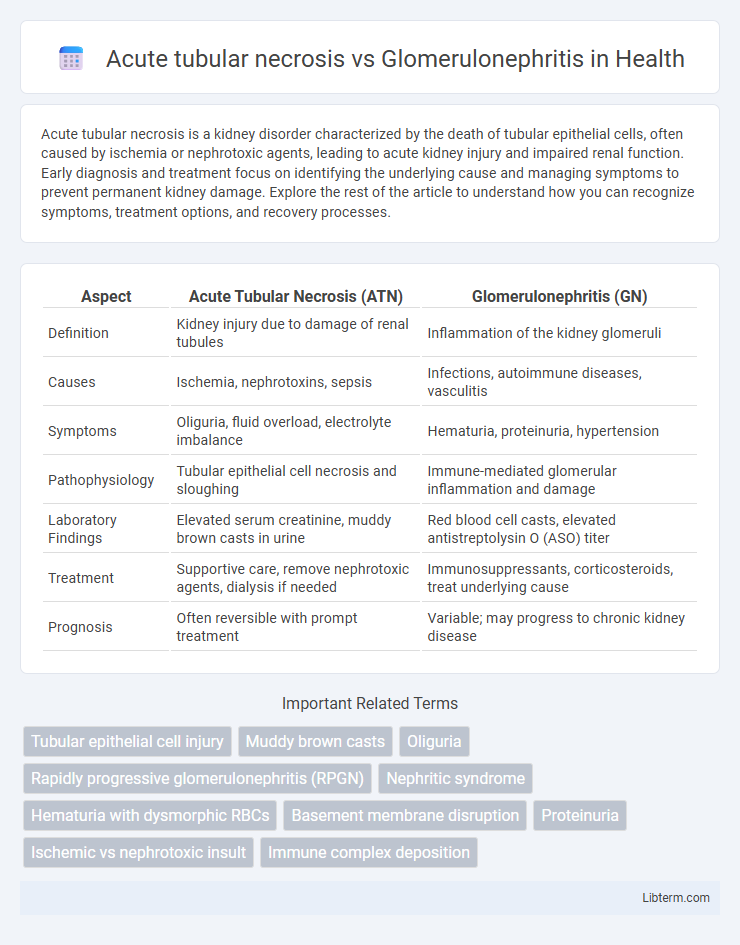
| Aspect | Acute Tubular Necrosis (ATN) | Glomerulonephritis (GN) |
|---|---|---|
| Definition | Kidney injury due to damage of renal tubules | Inflammation of the kidney glomeruli |
| Causes | Ischemia, nephrotoxins, sepsis | Infections, autoimmune diseases, vasculitis |
| Symptoms | Oliguria, fluid overload, electrolyte imbalance | Hematuria, proteinuria, hypertension |
| Pathophysiology | Tubular epithelial cell necrosis and sloughing | Immune-mediated glomerular inflammation and damage |
| Laboratory Findings | Elevated serum creatinine, muddy brown casts in urine | Red blood cell casts, elevated antistreptolysin O (ASO) titer |
| Treatment | Supportive care, remove nephrotoxic agents, dialysis if needed | Immunosuppressants, corticosteroids, treat underlying cause |
| Prognosis | Often reversible with prompt treatment | Variable; may progress to chronic kidney disease |
Introduction to Acute Tubular Necrosis and Glomerulonephritis
Acute tubular necrosis (ATN) involves the damage and death of tubular epithelial cells in the kidney, primarily caused by ischemia or nephrotoxic injury, leading to acute kidney injury. Glomerulonephritis refers to inflammation of the glomeruli, the kidney's filtering units, often triggered by autoimmune diseases, infections, or systemic conditions, resulting in impaired renal function and proteinuria. Differentiating ATN from glomerulonephritis relies on clinical presentation, laboratory findings, and kidney biopsy, which guide targeted treatment strategies.
Key Differences in Pathophysiology
Acute tubular necrosis (ATN) primarily involves ischemic or nephrotoxic injury to renal tubular epithelial cells, leading to tubular cell death and impaired kidney filtration. Glomerulonephritis is marked by immune-mediated inflammation of the glomeruli, causing damage to the glomerular basement membrane and resulting in proteinuria and hematuria. While ATN disrupts tubular function due to direct cellular injury, glomerulonephritis impairs glomerular filtration by inflammatory processes.
Etiology and Risk Factors
Acute tubular necrosis (ATN) primarily results from ischemic injury or nephrotoxins such as aminoglycosides, contrast agents, and sepsis-induced systemic hypotension, with risk factors including prolonged hypotension, major surgery, and pre-existing chronic kidney disease. In contrast, glomerulonephritis is caused by immune-mediated glomerular inflammation triggered by infections, autoimmune diseases like lupus erythematosus, and vasculitis, with risk factors comprising persistent infections, genetic predisposition, and systemic autoimmune disorders. Both conditions can lead to acute kidney injury but differ significantly in their underlying causes and associated predisposing factors.
Clinical Presentation and Symptoms
Acute tubular necrosis typically presents with sudden onset of oliguria or anuria, elevated serum creatinine, and symptoms related to uremia such as nausea and fatigue, often following ischemic or nephrotoxic insults. In contrast, glomerulonephritis commonly manifests with hematuria, proteinuria, edema, hypertension, and varying degrees of renal impairment depending on the severity and type of glomerular injury. Both conditions require careful clinical evaluation, but the presence of active urinary sediment and systemic symptoms may help differentiate glomerulonephritis from acute tubular necrosis.
Laboratory and Diagnostic Findings
Acute tubular necrosis (ATN) typically presents with elevated serum creatinine, muddy brown granular casts in urine sediment, and a low fractional excretion of sodium (FENa > 2%). In contrast, glomerulonephritis shows hematuria with dysmorphic red blood cells and red blood cell casts, along with proteinuria and often elevated anti-streptolysin O or anti-neutrophil cytoplasmic antibodies (ANCA) depending on the type. Renal biopsy in ATN reveals tubular epithelial cell necrosis, whereas glomerulonephritis demonstrates glomerular inflammation and immune complex deposition.
Urinalysis: ATN vs Glomerulonephritis
Urinalysis in acute tubular necrosis (ATN) typically reveals muddy brown granular casts and epithelial cell casts, indicating tubular injury, while urine generally shows mild proteinuria and is often non-nephrotic range. In glomerulonephritis, urinalysis demonstrates red blood cell (RBC) casts, dysmorphic RBCs, and significant proteinuria, often in the nephrotic range, reflecting glomerular inflammation and damage. The presence of complement levels or specific antibodies in serum further supports diagnosis when combined with urinalysis findings.
Histopathological Features
Acute tubular necrosis (ATN) is characterized histopathologically by diffuse tubular epithelial cell necrosis, loss of the brush border, tubular dilation, and granular casts within the lumens, particularly in the proximal tubules. Glomerulonephritis exhibits glomerular inflammation with hypercellularity, proliferative changes, capillary basement membrane thickening or disruption, and often immune complex deposition visible on immunofluorescence or electron microscopy. While ATN primarily affects tubular structures, glomerulonephritis primarily targets glomeruli, reflecting distinct pathological mechanisms and diagnostic features.
Management and Treatment Strategies
Management of acute tubular necrosis (ATN) primarily involves supportive care, including fluid balance optimization, avoidance of nephrotoxic agents, and renal replacement therapy when indicated to manage electrolyte imbalances and volume overload. Treatment strategies for glomerulonephritis focus on immunosuppressive therapy tailored to the specific type, such as corticosteroids, cyclophosphamide, or rituximab, alongside antihypertensive agents like ACE inhibitors or ARBs to reduce proteinuria and control blood pressure. Both conditions require precise diagnosis through laboratory tests and kidney biopsy to guide effective therapeutic interventions and prevent progression to chronic kidney disease.
Prognosis and Potential Complications
Acute tubular necrosis (ATN) generally has a favorable prognosis with appropriate and timely supportive care, often leading to reversible kidney injury and recovery of renal function within weeks. In contrast, glomerulonephritis prognosis varies widely depending on the underlying cause, with some forms progressing to chronic kidney disease or end-stage renal failure if untreated. Potential complications of ATN include persistent renal dysfunction and fluid overload, while glomerulonephritis may lead to complications such as nephrotic syndrome, hypertension, and irreversible glomerular scarring.
Summary and Key Takeaways
Acute tubular necrosis (ATN) primarily results from ischemic or toxic injury to renal tubules, leading to acute kidney injury characterized by decreased urine output and elevated serum creatinine. Glomerulonephritis involves inflammation of the glomeruli, often immune-mediated, causing hematuria, proteinuria, and variable renal impairment. Differentiating ATN from glomerulonephritis relies on clinical presentation, urine findings, and biopsy, with ATN showing tubular epithelial cell injury and glomerulonephritis revealing glomerular inflammation.
Acute tubular necrosis Infographic
 libterm.com
libterm.com