Severe hemolysis results in the rapid destruction of red blood cells, causing symptoms such as fatigue, jaundice, and dark urine. Recognizing the underlying causes like autoimmune disorders, infections, or medication reactions is crucial for timely treatment. Explore the rest of the article to understand how you can identify and manage severe hemolysis effectively.
Table of Comparison
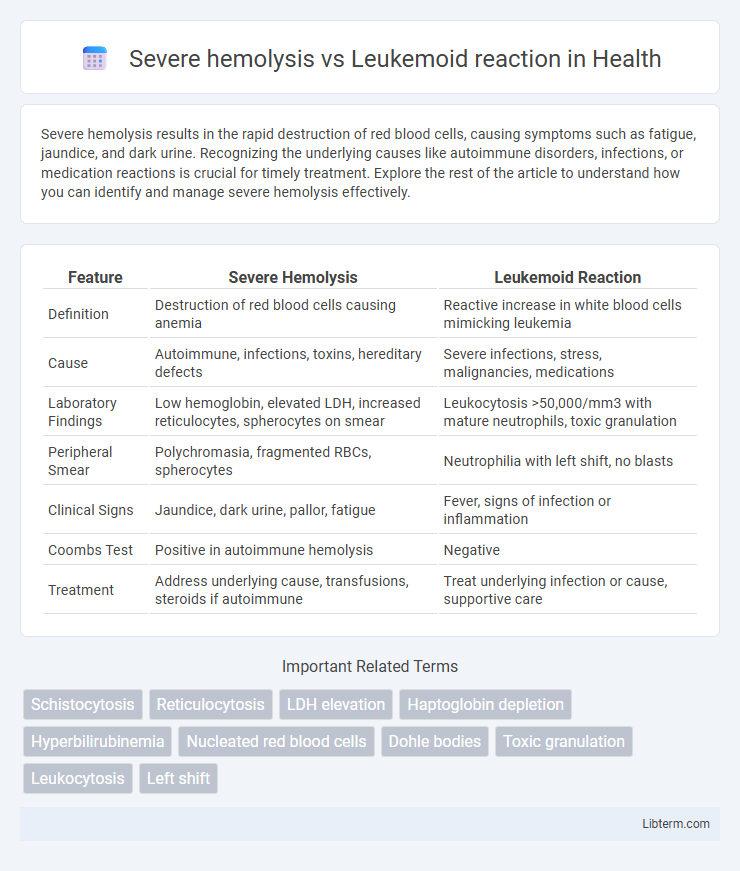
| Feature | Severe Hemolysis | Leukemoid Reaction |
|---|---|---|
| Definition | Destruction of red blood cells causing anemia | Reactive increase in white blood cells mimicking leukemia |
| Cause | Autoimmune, infections, toxins, hereditary defects | Severe infections, stress, malignancies, medications |
| Laboratory Findings | Low hemoglobin, elevated LDH, increased reticulocytes, spherocytes on smear | Leukocytosis >50,000/mm3 with mature neutrophils, toxic granulation |
| Peripheral Smear | Polychromasia, fragmented RBCs, spherocytes | Neutrophilia with left shift, no blasts |
| Clinical Signs | Jaundice, dark urine, pallor, fatigue | Fever, signs of infection or inflammation |
| Coombs Test | Positive in autoimmune hemolysis | Negative |
| Treatment | Address underlying cause, transfusions, steroids if autoimmune | Treat underlying infection or cause, supportive care |
Introduction to Severe Hemolysis and Leukemoid Reaction
Severe hemolysis involves the rapid destruction of red blood cells leading to anemia, elevated bilirubin, and increased lactate dehydrogenase (LDH). Leukemoid reaction presents as an extreme leukocytosis resembling leukemia but is a reactive process to infections or stress. Differentiating these conditions requires clinical context and laboratory evaluation of blood smears, reticulocyte counts, and inflammatory markers.
Definition and Key Features
Severe hemolysis is characterized by the rapid destruction of red blood cells leading to anemia, jaundice, and elevated lactate dehydrogenase (LDH) levels, whereas leukemoid reaction is a reactive leukocytosis mimicking leukemia with a white blood cell count often exceeding 50,000/uL and presence of immature granulocytes. Key features of severe hemolysis include reticulocytosis, decreased haptoglobin, and indirect hyperbilirubinemia, while leukemoid reaction presents with a marked neutrophilic leukocytosis, toxic granulations, and an absent leukemic blast population. Both conditions require differential diagnosis using clinical history, peripheral blood smear, and relevant laboratory markers to guide appropriate management.
Etiology: Causes of Severe Hemolysis vs Leukemoid Reaction
Severe hemolysis is primarily caused by autoimmune disorders, infections such as malaria, certain medications, or inherited conditions like sickle cell anemia and glucose-6-phosphate dehydrogenase (G6PD) deficiency. Leukemoid reaction results from severe infections, malignancies, or stress conditions like major hemorrhage or intoxications, triggering an excessive leukocyte response that mimics leukemia. Understanding the distinct etiologies is crucial for accurate diagnosis, as hemolysis involves red blood cell destruction, while leukemoid reaction involves reactive white blood cell proliferation.
Clinical Presentation: Symptoms and Signs
Severe hemolysis presents with symptoms including jaundice, dark urine, pallor, fatigue, and tachycardia due to rapid red blood cell destruction leading to anemia and elevated bilirubin levels. Leukemoid reaction is characterized by fever, malaise, and signs of systemic infection or inflammation, accompanied by extreme leukocytosis with a marked left shift and mature neutrophilia on peripheral smear. Both conditions may exhibit splenomegaly, but severe hemolysis often shows signs of hemolytic anemia while leukemoid reaction mimics leukemia with high white blood cell counts without blasts.
Hematological Findings and Laboratory Markers
Severe hemolysis is characterized by marked anemia, elevated reticulocyte count, increased lactate dehydrogenase (LDH), decreased haptoglobin, and elevated indirect bilirubin, reflecting accelerated red blood cell destruction. Leukemoid reaction presents with extreme leukocytosis, often exceeding 50,000 cells/mL, a left shift with increased neutrophil precursors, and elevated alkaline phosphatase levels, distinguishing it from malignant leukemias. Peripheral blood smear in hemolysis reveals schistocytes and spherocytes, while leukemoid reaction shows toxic granulation and Dohle bodies in neutrophils.
Pathophysiological Mechanisms
Severe hemolysis involves rapid destruction of red blood cells leading to the release of hemoglobin into the bloodstream, triggering oxidative stress and activating macrophage-mediated clearance in the spleen. Leukemoid reaction is characterized by an exaggerated white blood cell response, primarily neutrophilia, due to increased production and release of immature granulocytes from the bone marrow driven by inflammatory cytokines such as granulocyte colony-stimulating factor (G-CSF). The pathophysiological mechanisms differ fundamentally: hemolysis centers on erythrocyte membrane disruption and hemoglobin toxicity, while leukemoid reaction involves hyperactivation of bone marrow myelopoiesis in response to severe infection or inflammation.
Diagnostic Criteria and Differential Diagnosis
Severe hemolysis is characterized by elevated lactate dehydrogenase (LDH), decreased haptoglobin, increased indirect bilirubin, and reticulocytosis, indicating rapid red blood cell destruction. Leukemoid reaction presents with a marked leukocytosis, often exceeding 50,000 cells/uL, left shift with immature granulocytes, and high leukocyte alkaline phosphatase (LAP) score, distinguishing it from chronic myeloid leukemia. Differential diagnosis hinges on peripheral blood smear evaluation, Coombs test for hemolysis, and bone marrow examination to rule out leukemia or infection-related leukemoid response.
Complications and Prognostic Implications
Severe hemolysis can lead to complications such as acute kidney injury, disseminated intravascular coagulation, and severe anemia, which significantly worsen the prognosis if not promptly managed. Leukemoid reaction, characterized by an extreme leukocytosis often in response to infection or stress, typically has reversible outcomes but can mask underlying malignancies or severe infections, complicating diagnosis and treatment. Prognostic implications in severe hemolysis largely depend on the rapidity of onset and the effectiveness of hemolysis control, whereas leukemoid reactions require careful differentiation from leukemia to guide appropriate therapy and improve patient outcomes.
Management Strategies and Treatment Options
Severe hemolysis requires prompt management with blood transfusions and corticosteroids to reduce immune-mediated red cell destruction, while addressing underlying causes such as infections or autoimmune disorders. Leukemoid reaction treatment focuses on identifying and resolving the primary cause, often infection or inflammation, supported by antibiotics or anti-inflammatory agents, without the use of chemotherapeutic drugs typical for leukemia. Monitoring hematologic parameters and supportive care, including hydration and electrolyte balance, is essential in both conditions to prevent complications and promote recovery.
Summary: Key Differences and Clinical Considerations
Severe hemolysis involves rapid destruction of red blood cells leading to anemia, jaundice, and elevated LDH and indirect bilirubin, whereas leukemoid reaction presents as an extreme white blood cell increase caused by infections or stress, mimicking leukemia but with a benign underlying cause. Hemolysis typically shows a positive direct Coombs test and reticulocytosis, while leukemoid reaction features a high leukocyte alkaline phosphatase (LAP) score and absence of blasts. Clinical considerations include differentiating these conditions using laboratory markers to guide appropriate treatment, as hemolysis requires addressing the underlying cause of red cell destruction, while leukemoid reaction management focuses on resolving the inciting infection or inflammation.
Severe hemolysis Infographic
 libterm.com
libterm.com