Edema occurs when excess fluid accumulates in the body's tissues, leading to swelling and discomfort. Understanding the root causes, such as heart, kidney, or liver issues, is crucial for effective treatment and management. Explore the rest of the article to learn how you can identify symptoms and access appropriate care.
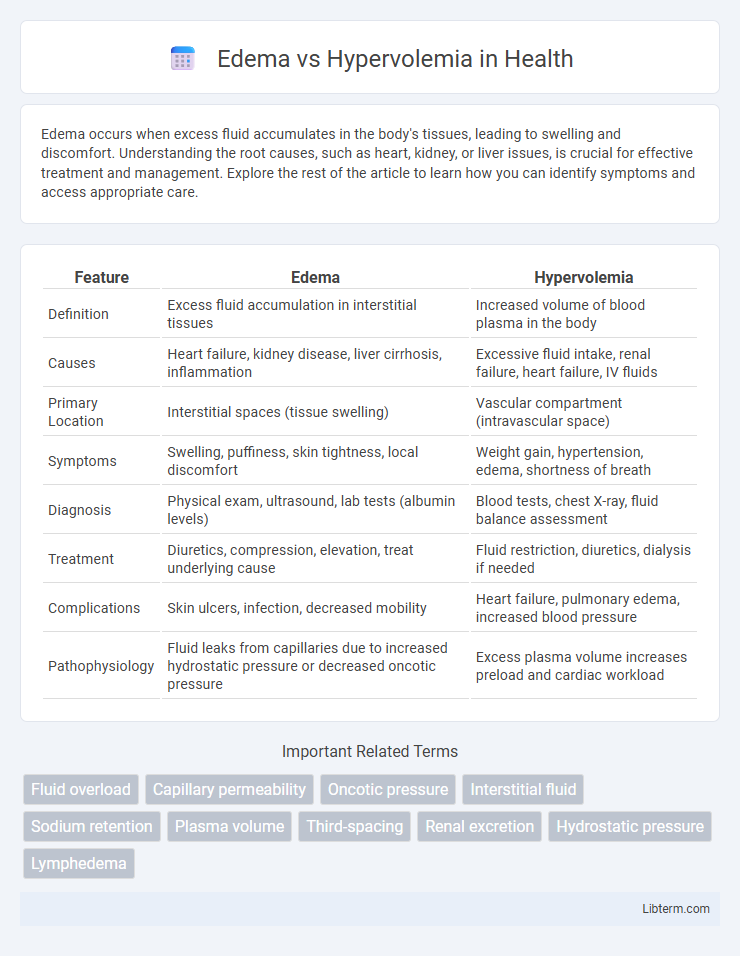
Table of Comparison
| Feature | Edema | Hypervolemia |
|---|---|---|
| Definition | Excess fluid accumulation in interstitial tissues | Increased volume of blood plasma in the body |
| Causes | Heart failure, kidney disease, liver cirrhosis, inflammation | Excessive fluid intake, renal failure, heart failure, IV fluids |
| Primary Location | Interstitial spaces (tissue swelling) | Vascular compartment (intravascular space) |
| Symptoms | Swelling, puffiness, skin tightness, local discomfort | Weight gain, hypertension, edema, shortness of breath |
| Diagnosis | Physical exam, ultrasound, lab tests (albumin levels) | Blood tests, chest X-ray, fluid balance assessment |
| Treatment | Diuretics, compression, elevation, treat underlying cause | Fluid restriction, diuretics, dialysis if needed |
| Complications | Skin ulcers, infection, decreased mobility | Heart failure, pulmonary edema, increased blood pressure |
| Pathophysiology | Fluid leaks from capillaries due to increased hydrostatic pressure or decreased oncotic pressure | Excess plasma volume increases preload and cardiac workload |
Understanding Edema: Definition and Causes
Edema is the abnormal accumulation of fluid in the interstitial spaces, leading to swelling, while hypervolemia refers to an increased volume of blood plasma within the circulatory system. Edema typically results from factors such as increased capillary hydrostatic pressure, decreased plasma oncotic pressure, lymphatic obstruction, or increased capillary permeability. Unlike hypervolemia, which involves excess intravascular fluid, edema primarily reflects extracellular fluid imbalance in tissues.
What is Hypervolemia? Key Characteristics
Hypervolemia is a medical condition characterized by an excessive increase in blood plasma volume, often caused by fluid retention or intravenous fluid administration. Key characteristics include swelling (edema), elevated blood pressure, rapid weight gain, and symptoms associated with congestive heart failure or kidney disease. Unlike edema, which is localized fluid accumulation in tissues, hypervolemia involves systemic fluid overload impacting cardiovascular function.
Edema vs Hypervolemia: Main Differences
Edema is the abnormal accumulation of fluid in the interstitial spaces causing tissue swelling, while hypervolemia refers to an increased volume of blood plasma in the vascular system. Edema primarily results from increased capillary permeability, lymphatic obstruction, or low plasma oncotic pressure, whereas hypervolemia often stems from fluid retention due to kidney dysfunction or heart failure. Clinically, edema presents as localized or generalized swelling, whereas hypervolemia may cause systemic symptoms such as hypertension and pulmonary congestion.
Common Symptoms of Edema
Edema commonly presents with localized swelling, particularly in the lower extremities, along with skin that appears stretched and shiny. Patients may experience discomfort or a sensation of heaviness in the affected areas, often worsening after prolonged standing or sitting. In contrast, hypervolemia involves an overall increase in blood volume and may produce symptoms like hypertension and rapid weight gain rather than the localized swelling seen in edema.
Identifying Symptoms of Hypervolemia
Hypervolemia presents with symptoms such as rapid weight gain, edema primarily in the lower extremities, and elevated blood pressure. Patients may also exhibit jugular vein distension, shortness of breath due to pulmonary congestion, and increased urine output. Early recognition of these clinical signs is crucial for managing fluid overload and preventing complications like heart failure.
Underlying Mechanisms: Fluid Retention Explained
Edema results from excessive fluid accumulation in the interstitial space due to increased capillary hydrostatic pressure, decreased plasma oncotic pressure, or lymphatic obstruction. Hypervolemia involves an overall increase in intravascular fluid volume caused by sodium and water retention primarily driven by renal pathologies, heart failure, or hormonal imbalances like aldosterone and antidiuretic hormone dysregulation. Both conditions share fluid retention but differ in their compartmental distribution and underlying pathophysiological mechanisms.
Risk Factors for Edema and Hypervolemia
Risk factors for edema include chronic venous insufficiency, heart failure, kidney disease, liver cirrhosis, and prolonged immobility, all of which disrupt normal fluid balance and cause fluid accumulation in tissues. Hypervolemia risk factors primarily involve excessive sodium and water intake, renal failure, congestive heart failure, and cirrhosis, leading to increased blood volume and vascular congestion. Both conditions often overlap in patients with compromised cardiac or renal function, exacerbating fluid retention complications.
Diagnostic Approaches: Distinguishing the Conditions
Diagnostic approaches for edema versus hypervolemia involve evaluating fluid distribution and volume status through clinical examination and laboratory tests. Edema is primarily identified by localized or generalized swelling with normal or low blood volume, whereas hypervolemia presents with increased total body fluid volume, evident in weight gain, elevated central venous pressure, and diluted blood tests. Imaging techniques such as ultrasound and chest X-rays assist in detecting fluid overload in hypervolemia, while serum electrolyte analysis and renal function tests help differentiate between the two conditions based on underlying causes.
Treatment Strategies: Edema vs Hypervolemia
Treatment strategies for edema primarily involve diuretics to remove excess fluid and addressing the underlying cause such as heart failure, liver cirrhosis, or kidney disease. Hypervolemia management includes sodium restriction, intravenous diuretics, and careful monitoring of fluid intake to prevent complications like pulmonary edema. Both conditions require close clinical assessment to tailor interventions effectively and avoid electrolyte imbalances.
Prevention and Management Tips for Fluid Imbalances
Preventing edema and hypervolemia involves maintaining a balanced diet low in sodium and monitoring fluid intake to avoid excessive volume overload. Regular physical activity and elevating affected limbs enhance venous return, reducing fluid accumulation in tissues. For management, diuretics prescribed by healthcare providers help eliminate excess fluid, while monitoring body weight daily assists in early detection of fluid retention.
Edema Infographic
 libterm.com
libterm.com