Pneumothorax occurs when air leaks into the space between your lung and chest wall, causing lung collapse and sudden chest pain or shortness of breath. Prompt diagnosis and treatment are crucial to prevent complications and restore normal lung function. Explore the rest of the article to understand the types, symptoms, causes, and effective management of pneumothorax.
Table of Comparison
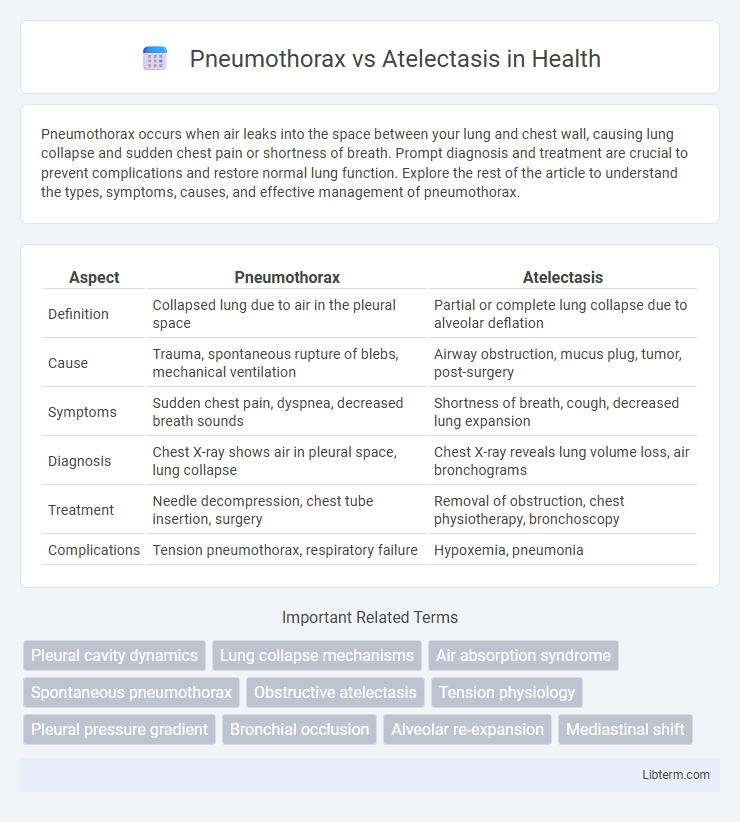
| Aspect | Pneumothorax | Atelectasis |
|---|---|---|
| Definition | Collapsed lung due to air in the pleural space | Partial or complete lung collapse due to alveolar deflation |
| Cause | Trauma, spontaneous rupture of blebs, mechanical ventilation | Airway obstruction, mucus plug, tumor, post-surgery |
| Symptoms | Sudden chest pain, dyspnea, decreased breath sounds | Shortness of breath, cough, decreased lung expansion |
| Diagnosis | Chest X-ray shows air in pleural space, lung collapse | Chest X-ray reveals lung volume loss, air bronchograms |
| Treatment | Needle decompression, chest tube insertion, surgery | Removal of obstruction, chest physiotherapy, bronchoscopy |
| Complications | Tension pneumothorax, respiratory failure | Hypoxemia, pneumonia |
Introduction to Pneumothorax and Atelectasis
Pneumothorax is the presence of air in the pleural space causing lung collapse, often resulting from trauma or spontaneous rupture of lung blebs. Atelectasis involves the partial or complete collapse of lung tissue due to airway obstruction, compression, or surfactant deficiency, leading to impaired gas exchange. Both conditions present with respiratory distress but differ in pathophysiology and management strategies.
Definition and Overview
Pneumothorax is the presence of air in the pleural cavity causing lung collapse, while atelectasis refers to the partial or complete collapse of lung tissue due to alveolar deflation. Pneumothorax often results from trauma or spontaneous rupture of lung blebs, leading to impaired lung expansion and respiratory distress. Atelectasis can arise from airway obstruction, compression, or surfactant deficiency, reducing gas exchange efficiency and causing hypoxemia.
Causes and Risk Factors
Pneumothorax occurs due to air entering the pleural space, often caused by chest trauma, spontaneous rupture of lung blebs, or underlying lung diseases like COPD. Atelectasis results from airway obstruction, lung compression, or surfactant deficiency, frequently linked to postoperative complications, mucus plugs, or prolonged immobility. Risk factors for pneumothorax include smoking, asthma, and tall, thin body habitus, while atelectasis risk increases with lung infections, anesthesia, and severe chest injuries.
Pathophysiology of Pneumothorax
Pneumothorax occurs when air enters the pleural space, causing a loss of negative pressure and leading to lung collapse due to the inability of the lung to expand. This disruption in the pleural pressure gradient impairs ventilation and decreases oxygen exchange, resulting in respiratory distress. In contrast, atelectasis involves the collapse of alveoli due to obstruction, compression, or surfactant deficiency, but the pleural space remains intact.
Pathophysiology of Atelectasis
Atelectasis involves the collapse or incomplete expansion of lung tissue, primarily caused by obstruction of the airways or external compression preventing alveolar ventilation. The pathophysiology includes surfactant deficiency, airway obstruction by mucus plugs or foreign bodies, and compression from pleural effusions or tumors, leading to impaired gas exchange and hypoxemia. In contrast to pneumothorax, which is characterized by air in the pleural space causing lung collapse, atelectasis results from impaired alveolar inflation without pleural air involvement.
Clinical Presentation and Symptoms
Pneumothorax typically presents with sudden onset of sharp, unilateral chest pain and acute shortness of breath, often accompanied by decreased breath sounds and hyperresonance on the affected side during physical examination. In contrast, atelectasis manifests with gradual or sudden onset of dyspnea, cough, and decreased breath sounds, along with dullness to percussion and reduced chest expansion on the involved lung segment. Both conditions can cause hypoxemia, but the presence of tracheal deviation and hemodynamic instability is more characteristic of tension pneumothorax, requiring urgent intervention.
Diagnostic Approaches
Chest X-ray remains the cornerstone for distinguishing pneumothorax from atelectasis, revealing air in the pleural space or lung collapse respectively. Computed tomography (CT) provides enhanced visualization, accurately identifying subtle pneumothorax and differentiating atelectasis patterns caused by obstruction or compression. Ultrasonography, particularly lung ultrasound, detects the absence of lung sliding in pneumothorax and identifies consolidated lung tissue consistent with atelectasis.
Radiological Differences
Pneumothorax appears on radiographs as a visible pleural line with absent lung markings peripheral to this line, indicating air in the pleural space causing lung collapse. Atelectasis demonstrates increased lung opacity due to alveolar collapse and volume loss, often with shift of adjacent structures like the mediastinum or diaphragm toward the affected side. Key radiological differences include pneumothorax showing hyperlucency without lung markings, while atelectasis presents as areas of increased density with loss of normal lung volume.
Treatment and Management Strategies
Treatment of pneumothorax typically involves immediate intervention such as needle aspiration or chest tube insertion to remove air and re-expand the lung, with surgery considered for recurrent cases or persistent air leaks. Atelectasis management focuses on resolving underlying causes, using techniques like chest physiotherapy, incentive spirometry, and addressing airway obstruction to promote lung re-expansion. Both conditions require close monitoring through imaging and respiratory support to prevent complications and ensure effective lung function restoration.
Prognosis and Complications
Pneumothorax prognosis varies based on the size and underlying lung health, with spontaneous pneumothorax often resolving with minimal intervention but tension pneumothorax posing life-threatening risks requiring urgent treatment. Atelectasis prognosis depends on the cause and extent of lung collapse, often improving with prompt treatment addressing airway obstruction or underlying pathology, but prolonged atelectasis can lead to infection or respiratory failure. Complications of pneumothorax include respiratory distress, recurrence, and persistent air leaks, while atelectasis complications may involve pneumonia, hypoxemia, and impaired lung function.
Pneumothorax Infographic
 libterm.com
libterm.com