Xerostomia, commonly known as dry mouth, results from reduced saliva production and can lead to difficulties in speaking, swallowing, and increased dental decay risk. Managing xerostomia involves staying hydrated, using saliva substitutes, and avoiding irritants like alcohol and tobacco. Discover effective treatments and lifestyle tips in the rest of the article to improve your oral comfort and health.
Table of Comparison
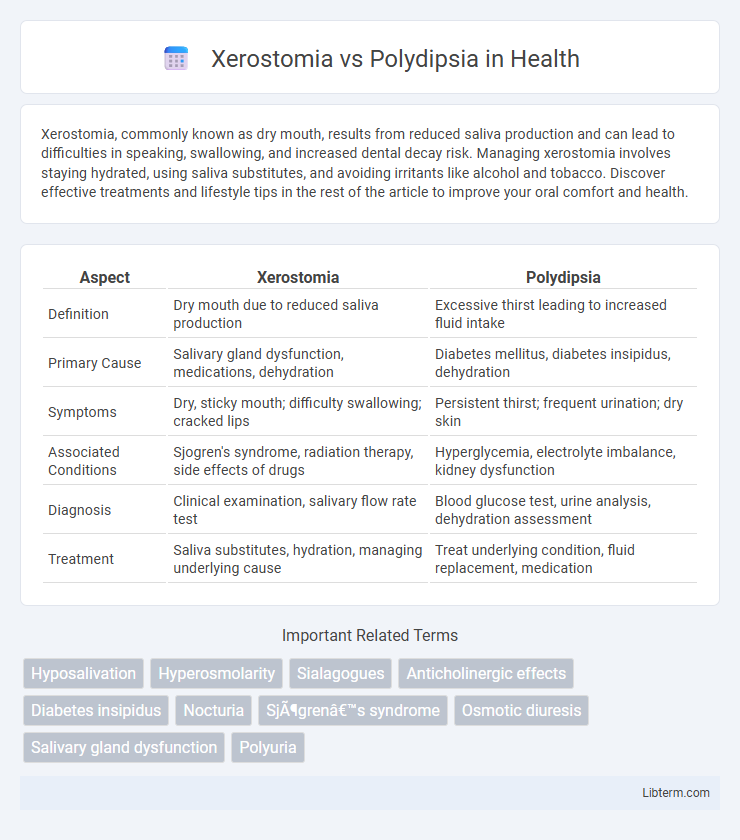
| Aspect | Xerostomia | Polydipsia |
|---|---|---|
| Definition | Dry mouth due to reduced saliva production | Excessive thirst leading to increased fluid intake |
| Primary Cause | Salivary gland dysfunction, medications, dehydration | Diabetes mellitus, diabetes insipidus, dehydration |
| Symptoms | Dry, sticky mouth; difficulty swallowing; cracked lips | Persistent thirst; frequent urination; dry skin |
| Associated Conditions | Sjogren's syndrome, radiation therapy, side effects of drugs | Hyperglycemia, electrolyte imbalance, kidney dysfunction |
| Diagnosis | Clinical examination, salivary flow rate test | Blood glucose test, urine analysis, dehydration assessment |
| Treatment | Saliva substitutes, hydration, managing underlying cause | Treat underlying condition, fluid replacement, medication |
Introduction to Xerostomia and Polydipsia
Xerostomia refers to the sensation of dry mouth caused by reduced or absent saliva flow, often linked to medications, autoimmune diseases like Sjogren's syndrome, or radiation therapy. Polydipsia is characterized by excessive thirst and fluid intake, commonly associated with conditions such as diabetes mellitus, diabetes insipidus, or certain psychiatric disorders. Understanding xerostomia and polydipsia involves recognizing their distinct etiologies and clinical implications within oral health and systemic hydration regulation.
Defining Xerostomia: Causes and Symptoms
Xerostomia, commonly known as dry mouth, results from decreased saliva production caused by factors such as medication side effects, autoimmune diseases like Sjogren's syndrome, radiation therapy, or dehydration. Symptoms include a sticky, dry sensation in the oral cavity, difficulty swallowing or speaking, and an increased risk of dental caries and oral infections. Unlike polydipsia, which involves excessive thirst and fluid intake, xerostomia specifically refers to the oral dryness affecting the mucous membranes and salivary gland function.
Understanding Polydipsia: Triggers and Manifestations
Polydipsia, characterized by excessive thirst and fluid intake, often arises from underlying conditions such as diabetes mellitus, dehydration, or psychological factors like psychogenic polydipsia. This excessive thirst results from the body's need to regulate blood osmolarity and maintain homeostasis, distinguishing it from xerostomia, which is the subjective sensation of dry mouth due to reduced saliva production. Recognizing the triggers and manifestations of polydipsia is crucial for accurate diagnosis and effective treatment, as it can lead to electrolyte imbalances and affect overall health.
Key Differences Between Xerostomia and Polydipsia
Xerostomia refers to the subjective sensation of dry mouth caused by reduced or absent saliva flow, often linked to conditions like Sjogren's syndrome or medication side effects. Polydipsia is characterized by excessive thirst and fluid intake, commonly associated with diabetes mellitus or psychogenic causes. The key difference lies in xerostomia being a symptom of decreased saliva production leading to dry oral mucosa, while polydipsia involves hyperhydration behavior resulting from systemic imbalances affecting fluid regulation.
Shared Risk Factors and Overlapping Symptoms
Xerostomia and polydipsia share common risk factors such as diabetes mellitus, medication side effects (particularly from antihypertensives and anticholinergics), and dehydration. Both conditions frequently present with overlapping symptoms including dry mouth, increased thirst, and difficulty swallowing, complicating differential diagnosis. Understanding these shared etiologies and clinical manifestations is critical for accurate assessment and effective management of underlying metabolic or systemic disorders.
Diagnostic Approaches for Xerostomia vs Polydipsia
Diagnostic approaches for xerostomia primarily involve salivary flow rate measurement, oral examination, and assessment of underlying causes such as Sjogren's syndrome or medication side effects. Polydipsia evaluation includes detailed patient history, blood tests for glucose levels to rule out diabetes mellitus, and water deprivation tests to differentiate between primary polydipsia and diabetes insipidus. Imaging and biochemical analyses aid in confirming diagnoses by targeting specific pathophysiological mechanisms behind xerostomia or polydipsia.
Impact on Oral and Systemic Health
Xerostomia, characterized by dry mouth due to reduced saliva production, significantly increases the risk of dental caries, oral infections, and mucosal discomfort, impairing oral health and overall quality of life. Polydipsia, marked by excessive thirst and fluid intake, often signals underlying systemic conditions such as diabetes mellitus, which can exacerbate oral complications including periodontal disease and delayed wound healing. Both conditions necessitate targeted management to prevent adverse outcomes on oral mucosa integrity and systemic metabolic balance.
Effective Treatment Options for Xerostomia
Xerostomia, characterized by dry mouth due to reduced saliva production, requires targeted treatments such as saliva substitutes, pilocarpine, and cevimeline to stimulate salivary flow and improve oral moisture. Polydipsia, excessive thirst often related to underlying conditions like diabetes or psychogenic disorders, demands management of the root cause rather than symptom-specific therapies. Effective treatment options for xerostomia include hydrating oral gels, sugar-free chewing gums, and proper oral hygiene practices to prevent complications like dental caries and oral infections.
Management Strategies for Polydipsia
Management strategies for polydipsia focus on addressing the underlying cause, often involving behavioral modification and medical intervention. Fluid intake regulation through scheduled drinking routines helps prevent excessive water consumption and associated complications like hyponatremia. Healthcare providers may also monitor electrolyte levels and prescribe medications such as antipsychotics or desmopressin when polydipsia is linked to psychiatric conditions or diabetes insipidus.
Preventive Measures and Lifestyle Modifications
Xerostomia prevention emphasizes maintaining proper oral hygiene, staying hydrated, and avoiding tobacco or alcohol, which can exacerbate dry mouth symptoms. Polydipsia management focuses on monitoring fluid intake, treating underlying conditions such as diabetes or psychiatric disorders, and implementing dietary modifications to balance electrolyte levels. Both conditions benefit from regular medical evaluations and personalized lifestyle adjustments to reduce symptom severity and improve quality of life.
Xerostomia Infographic
 libterm.com
libterm.com