A hematoma is a localized collection of blood outside the blood vessels, usually caused by injury or trauma that leads to blood vessel rupture. Symptoms can include swelling, pain, bruising, and limited mobility depending on the size and location of the hematoma. To learn more about causes, treatment options, and when to seek medical attention, continue reading the rest of the article.
Table of Comparison
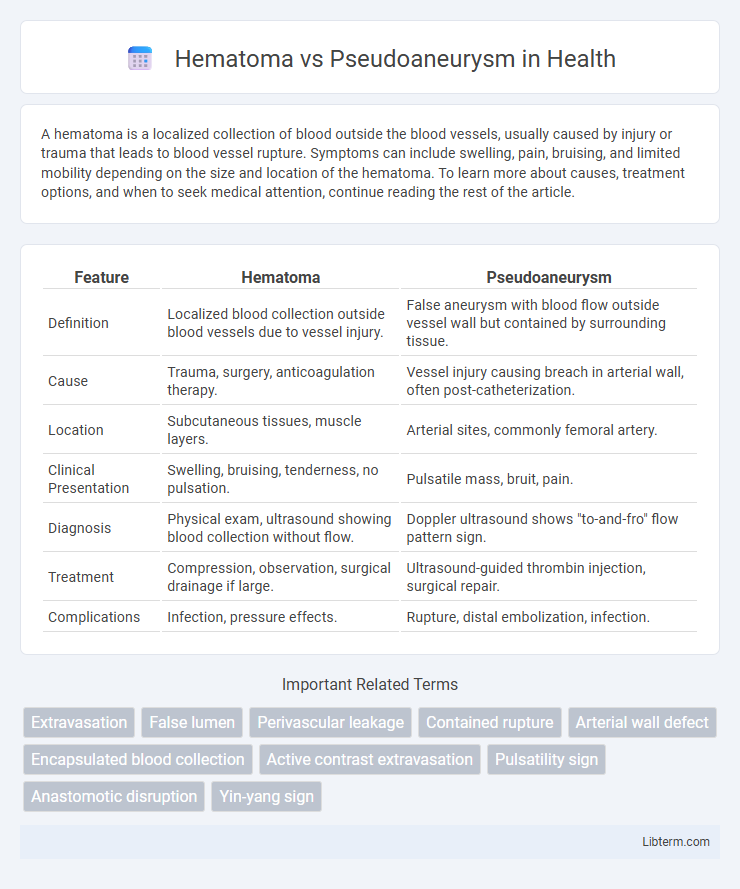
| Feature | Hematoma | Pseudoaneurysm |
|---|---|---|
| Definition | Localized blood collection outside blood vessels due to vessel injury. | False aneurysm with blood flow outside vessel wall but contained by surrounding tissue. |
| Cause | Trauma, surgery, anticoagulation therapy. | Vessel injury causing breach in arterial wall, often post-catheterization. |
| Location | Subcutaneous tissues, muscle layers. | Arterial sites, commonly femoral artery. |
| Clinical Presentation | Swelling, bruising, tenderness, no pulsation. | Pulsatile mass, bruit, pain. |
| Diagnosis | Physical exam, ultrasound showing blood collection without flow. | Doppler ultrasound shows "to-and-fro" flow pattern sign. |
| Treatment | Compression, observation, surgical drainage if large. | Ultrasound-guided thrombin injection, surgical repair. |
| Complications | Infection, pressure effects. | Rupture, distal embolization, infection. |
Understanding Hematoma: Definition and Causes
A hematoma is a localized collection of blood outside blood vessels, usually caused by trauma, surgery, or vascular injury leading to vessel rupture and blood pooling in surrounding tissues. It often appears as a swollen, painful mass and may vary in severity depending on the size and location of the bleeding. Common causes include blunt force trauma, anticoagulant therapy complications, and invasive medical procedures that compromise vessel integrity.
What is a Pseudoaneurysm? Key Features and Origins
A pseudoaneurysm, also known as a false aneurysm, occurs when a blood vessel wall is injured and blood leaks into the surrounding tissue, forming a hematoma that remains in communication with the arterial lumen. Unlike a true aneurysm, which involves all three layers of the vessel wall, a pseudoaneurysm lacks an intact vessel wall and is contained by the adventitia or surrounding perivascular tissue. Key features include a pulsatile mass, turbulent blood flow detectable by Doppler ultrasound, and a neck connecting the hematoma to the artery, often arising from trauma, catheterization procedures, or vascular surgery complications.
Pathophysiology: Hematoma vs Pseudoaneurysm
Hematoma forms when blood leaks from a damaged vessel into surrounding tissues, creating a localized collection of clotted blood confined by tissue planes. Pseudoaneurysm results from a breach in the arterial wall leading to blood flow outside the vessel lumen, contained only by the adventitia or periarterial tissue, forming a pulsatile sac connected to the artery. Unlike hematomas, pseudoaneurysms maintain communication with the arterial lumen, posing a higher risk of expansion and rupture due to persistent arterial pressure.
Risk Factors Associated with Hematomas and Pseudoaneurysms
Risk factors associated with hematomas include trauma, anticoagulant therapy, and invasive medical procedures that cause vessel injury or bleeding into soft tissues. Pseudoaneurysms often result from arterial puncture, catheterization, or surgical interventions, with increased risk in patients with hypertension, arteriosclerosis, or connective tissue disorders. Both conditions are influenced by underlying vessel fragility and coagulation abnormalities, which contribute to their development and complications.
Clinical Presentation: Symptoms and Signs
Hematomas typically present as localized swelling, pain, and skin discoloration at the injury site, often accompanied by tenderness and limited movement due to blood accumulation in tissues. Pseudoaneurysms manifest with pulsatile masses, palpable thrills, and audible bruits over affected arteries, frequently causing localized pain and potential distal ischemic symptoms if arterial flow is compromised. Both conditions require careful clinical examination and imaging to differentiate based on vascular involvement and symptom characteristics.
Diagnostic Approaches: Imaging and Differentiation
Diagnostic imaging plays a crucial role in differentiating hematoma from pseudoaneurysm. Ultrasound with Doppler can identify a pseudoaneurysm by detecting turbulent, pulsatile blood flow within the sac, whereas a hematoma typically appears as a non-vascular, hypoechoic collection. Computed tomography angiography (CTA) and magnetic resonance imaging (MRI) provide detailed visualization of vessel walls and surrounding tissues, enhancing differentiation by showing active contrast extravasation in pseudoaneurysms compared to the static, localized blood collection seen in hematomas.
Treatment Options: Hematoma Management Strategies
Hematoma management primarily involves conservative treatments such as rest, ice compression, and elevation to reduce swelling and promote natural reabsorption. In cases where the hematoma is large or causing significant pain, aspiration or surgical evacuation may be necessary to prevent complications. Monitoring for infection and ensuring proper wound care are essential components to optimize recovery outcomes.
Approaches to Treating Pseudoaneurysms
Treatment of pseudoaneurysms typically involves ultrasound-guided compression therapy, thrombin injection, or surgical repair, depending on the size and location of the lesion. Ultrasound-guided thrombin injection has become the preferred minimally invasive method due to its high success rate and low complication risk. Surgical intervention is reserved for pseudoaneurysms that fail less invasive treatments or those with risk of rupture or significant symptoms.
Complications and Prognosis: What to Expect
Hematomas often resolve with conservative treatment but can lead to complications such as infection, nerve compression, or chronic pain if untreated. Pseudoaneurysms carry a higher risk of rupture, thrombosis, and distal embolization, requiring prompt intervention to avoid serious vascular compromise. Prognosis varies: hematomas generally have a favorable outcome with proper care, whereas pseudoaneurysms demand close monitoring and potentially surgical or endovascular repair for optimal recovery.
Prevention and Patient Education
Proper wound care and avoiding excessive pressure or trauma at puncture sites significantly reduce the risk of hematoma formation after catheterization or injections. Educating patients on recognizing early signs such as swelling, bruising, or pulsatile masses enables prompt medical evaluation to differentiate hematoma from pseudoaneurysm. Emphasizing adherence to post-procedure instructions and timely follow-up minimizes complications and promotes effective management of vascular access sites.
Hematoma Infographic
 libterm.com
libterm.com