Nocturia is a condition characterized by waking up multiple times at night to urinate, which can disrupt sleep and affect overall quality of life. It is commonly caused by factors such as aging, increased fluid intake before bedtime, or underlying medical conditions like urinary tract infections or diabetes. Discover how you can manage nocturia effectively by exploring treatment options and lifestyle changes in the rest of this article.
Table of Comparison
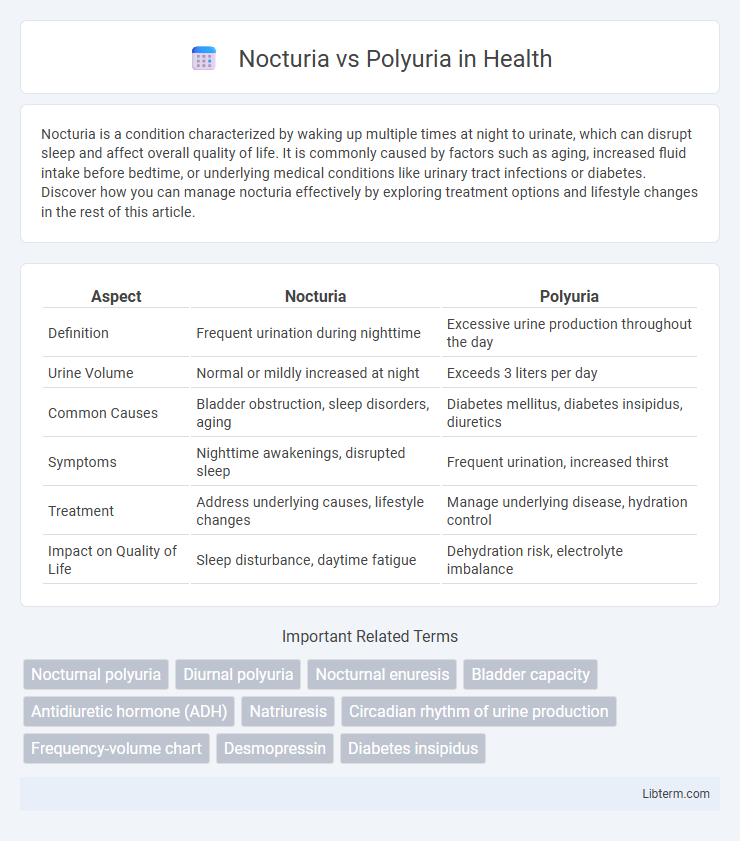
| Aspect | Nocturia | Polyuria |
|---|---|---|
| Definition | Frequent urination during nighttime | Excessive urine production throughout the day |
| Urine Volume | Normal or mildly increased at night | Exceeds 3 liters per day |
| Common Causes | Bladder obstruction, sleep disorders, aging | Diabetes mellitus, diabetes insipidus, diuretics |
| Symptoms | Nighttime awakenings, disrupted sleep | Frequent urination, increased thirst |
| Treatment | Address underlying causes, lifestyle changes | Manage underlying disease, hydration control |
| Impact on Quality of Life | Sleep disturbance, daytime fatigue | Dehydration risk, electrolyte imbalance |
Understanding Nocturia and Polyuria
Nocturia is characterized by the need to wake up one or more times during the night to urinate, often disrupting sleep quality. Polyuria involves the excessive production of urine, typically defined as more than 3 liters per day in adults, and can occur during both day and night. Differentiating between nocturia and polyuria is essential for diagnosing underlying conditions such as diabetes, bladder disorders, or sleep disturbances.
Key Differences Between Nocturia and Polyuria
Nocturia is characterized by the need to wake up one or more times during the night to urinate, whereas polyuria involves the excessive production of urine totaling more than 3 liters per day. Nocturia primarily affects sleep patterns and may result from bladder storage issues or systemic conditions like heart failure, while polyuria is often linked to disorders such as diabetes mellitus or diabetes insipidus causing increased diuresis. Understanding these distinct clinical features aids in accurate diagnosis and targeted treatment strategies for patients presenting with abnormal urination patterns.
Common Causes of Nocturia
Nocturia, characterized by frequent nighttime urination, is commonly caused by conditions such as benign prostatic hyperplasia (BPH), heart failure, diabetes mellitus, and sleep apnea. Polyuria, the excessive production of urine, often results from uncontrolled diabetes mellitus, diuretic use, or kidney disorders. Differentiating between nocturia due to increased urine production at night and polyuria involving total daily urine volume aids in accurate diagnosis and treatment.
Primary Causes of Polyuria
Polyuria primarily results from conditions that increase urine production, such as diabetes mellitus, where high blood glucose levels lead to osmotic diuresis. Another common cause is diabetes insipidus, characterized by impaired antidiuretic hormone (ADH) function, causing excessive water loss through urine. Excessive fluid intake, known as polydipsia, can also cause polyuria by overwhelming renal capacity to reabsorb water.
Symptoms: Nocturia vs. Polyuria
Nocturia primarily presents as frequent nighttime urination that disrupts sleep, with individuals waking multiple times during the night to urinate despite normal total daily urine volume. Polyuria is characterized by an excessive production of urine throughout the day, often exceeding 3 liters daily, leading to increased urination frequency both day and night. Differentiating symptoms include nocturia's focus on sleep interruption versus polyuria's overall increased urine output causing persistent thirst and dehydration risks.
Diagnostic Approaches for Nocturia and Polyuria
Diagnostic approaches for nocturia and polyuria involve detailed patient history and specific tests to distinguish underlying causes. Nocturia is evaluated through frequency volume charts, post-void residual urine measurement, and assessment for nocturnal polyuria using a nocturnal polyuria index. Polyuria diagnosis requires 24-hour urine volume quantification, serum glucose testing to rule out diabetes mellitus, and urine osmolality assessment to identify diabetes insipidus or osmotic diuresis.
Risk Factors and Associated Conditions
Nocturia is frequently linked to risk factors such as aging, obesity, diabetes mellitus, and cardiovascular diseases, which contribute to nighttime urine production and disrupted sleep. Polyuria is characterized by excessive urine output often caused by uncontrolled diabetes, diuretic use, or conditions like primary polydipsia and chronic kidney disease. Both conditions may coexist in patients with systemic disorders but require distinct diagnostic attention due to their different underlying pathophysiologies and management strategies.
Treatment Options: Nocturia
Nocturia treatment options include behavioral therapies such as fluid restriction before bedtime, bladder training, and pelvic floor muscle exercises tailored to reduce nighttime urination frequency. Pharmacological interventions often involve desmopressin, which decreases urine production, and anticholinergic drugs that improve bladder storage capacity. Addressing underlying medical conditions like sleep apnea, diabetes, or heart failure is essential for effective nocturia management and symptom relief.
Management Strategies for Polyuria
Polyuria management centers on identifying and treating underlying causes such as diabetes mellitus, diabetes insipidus, and excessive fluid intake. Pharmacologic interventions include desmopressin for central diabetes insipidus and optimizing glycemic control in diabetes mellitus to reduce urine volume. Lifestyle modifications entail restricting fluid intake before bedtime and avoiding diuretics, alongside regular monitoring of fluid balance and electrolyte levels to prevent complications.
Prevention Tips and Lifestyle Modifications
Nocturia and polyuria can be managed through targeted prevention tips and lifestyle modifications such as reducing evening fluid intake, limiting caffeine and alcohol consumption, and maintaining a healthy weight to reduce bladder pressure. Incorporating pelvic floor exercises, managing diabetes, and addressing sleep apnea are key strategies to control symptoms and improve nighttime urinary frequency. Regular monitoring of fluid balance and consulting a healthcare provider for underlying conditions enhances overall bladder health and prevents excessive urination episodes.
Nocturia Infographic
 libterm.com
libterm.com