Seizures result from sudden, abnormal electrical activity in the brain causing temporary disruptions in movement, sensation, or awareness. Understanding the types, triggers, and treatment options is crucial for effectively managing your condition and minimizing risks. Explore the rest of the article to learn how to recognize symptoms and support seizure control.
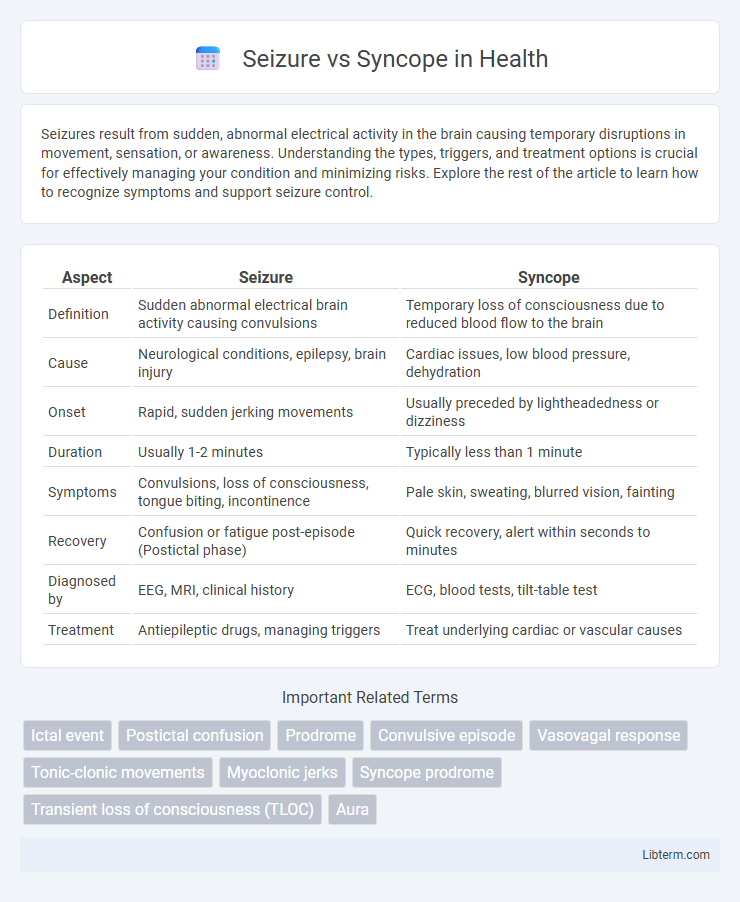
Table of Comparison
| Aspect | Seizure | Syncope |
|---|---|---|
| Definition | Sudden abnormal electrical brain activity causing convulsions | Temporary loss of consciousness due to reduced blood flow to the brain |
| Cause | Neurological conditions, epilepsy, brain injury | Cardiac issues, low blood pressure, dehydration |
| Onset | Rapid, sudden jerking movements | Usually preceded by lightheadedness or dizziness |
| Duration | Usually 1-2 minutes | Typically less than 1 minute |
| Symptoms | Convulsions, loss of consciousness, tongue biting, incontinence | Pale skin, sweating, blurred vision, fainting |
| Recovery | Confusion or fatigue post-episode (Postictal phase) | Quick recovery, alert within seconds to minutes |
| Diagnosed by | EEG, MRI, clinical history | ECG, blood tests, tilt-table test |
| Treatment | Antiepileptic drugs, managing triggers | Treat underlying cardiac or vascular causes |
Introduction to Seizure and Syncope
Seizures are sudden, abnormal electrical disturbances in the brain causing involuntary movements, sensory disruptions, or loss of consciousness. Syncope, also known as fainting, is a brief loss of consciousness due to reduced cerebral blood flow, often triggered by dehydration, low blood pressure, or cardiac issues. Differentiating seizures from syncope is critical for accurate diagnosis and treatment, as their causes, symptoms, and management differ significantly.
Defining Seizures: Causes and Mechanisms
Seizures are sudden, uncontrolled electrical disturbances in the brain that can alter behavior, movements, or consciousness. Causes include epilepsy, brain injury, infections, and metabolic imbalances, leading to abnormal neuronal firing and synchronization. The underlying mechanisms involve hyperexcitable neurons that disrupt normal brain signaling pathways, resulting in the characteristic convulsions or sensory disturbances.
Understanding Syncope: Causes and Mechanisms
Syncope, often referred to as fainting, results from a temporary reduction in cerebral blood flow causing brief loss of consciousness. Common causes include vasovagal episodes, cardiac arrhythmias, and orthostatic hypotension, each disrupting blood flow or autonomic regulation. Understanding these mechanisms helps differentiate syncope from seizures, which involve abnormal electrical activity in the brain rather than circulatory disturbances.
Key Differences Between Seizure and Syncope
Seizure and syncope differ primarily in their pathophysiology and clinical presentation; seizures result from abnormal electrical activity in the brain causing convulsions or loss of consciousness, while syncope is a transient loss of consciousness due to cerebral hypoperfusion often triggered by cardiac or vascular causes. Seizures typically involve prolonged postictal confusion and abnormal motor activity, whereas syncope features rapid full recovery with minimal confusion and no convulsions. Diagnostic tools such as EEG detect seizure activity, while ECG and tilt-table tests help identify syncope etiology, highlighting their distinct underlying mechanisms.
Signs and Symptoms: Seizure vs Syncope
Seizures typically present with sudden, involuntary muscle contractions, loss of consciousness, tongue biting, and postictal confusion, whereas syncope involves a brief loss of consciousness due to reduced cerebral blood flow, often preceded by lightheadedness, pallor, and sweating. Seizure signs include aura, convulsions, and incontinence, while syncope symptoms feature rapid recovery without confusion or muscle jerking. Differentiating these signs and symptoms is crucial for accurate diagnosis and appropriate treatment.
Diagnostic Approaches for Seizure and Syncope
Differentiating seizure from syncope relies heavily on detailed clinical history and diagnostic testing such as electroencephalography (EEG) for seizures and tilt table testing for syncope. Neuroimaging with MRI may assist in identifying structural brain abnormalities associated with seizures, while cardiovascular evaluation including ECG and echocardiography is crucial for syncope diagnosis. Biomarkers and ambulatory monitoring like Holter monitors further aid in distinguishing between epileptic events and cardiac-related transient loss of consciousness.
Risk Factors and Triggers Comparison
Seizure risk factors include epilepsy, brain injury, infections, and genetic predisposition, while syncope is often triggered by cardiovascular issues like arrhythmias, orthostatic hypotension, and vasovagal responses. Seizure triggers commonly involve sleep deprivation, flashing lights, and stress, contrasting with syncope triggers such as dehydration, prolonged standing, and sudden postural changes. Differentiating these conditions based on risk profiles and precipitating factors is crucial for accurate diagnosis and management.
Treatment Strategies: Seizure vs Syncope
Treatment strategies for seizures often involve anticonvulsant medications such as levetiracetam or valproate to control abnormal electrical brain activity, along with lifestyle modifications and epilepsy surgery in refractory cases. Syncope treatment prioritizes identifying and managing underlying causes like arrhythmias or vasovagal triggers, using interventions such as pacemaker implantation for cardiac causes or increased salt and fluid intake for neurocardiogenic syncope. Both conditions require tailored approaches involving diagnostic evaluations like EEG for seizures and tilt-table testing for syncope to guide effective management plans.
Prevention and Management Tips
Seizure prevention involves identifying triggers such as sleep deprivation, stress, and medication noncompliance, while management includes antiepileptic drugs tailored to seizure type and lifestyle modifications to reduce risk factors. Syncope prevention emphasizes controlling underlying causes like dehydration, orthostatic hypotension, or arrhythmias through hydration, electrolyte balance, and cardiovascular evaluation. Both conditions require patient education on symptom recognition and prompt medical consultation to optimize outcomes and reduce recurrence.
When to Seek Medical Attention
Seek immediate medical attention if a seizure lasts more than five minutes, occurs repeatedly without recovery, or is accompanied by difficulty breathing, injury, or loss of consciousness. Syncope requires prompt evaluation when fainting is sudden, recurrent, occurs during exertion, or is associated with chest pain, palpitations, or neurological symptoms. Timely diagnosis of seizure or syncope is critical to prevent complications and determine appropriate treatment.
Seizure Infographic
 libterm.com
libterm.com