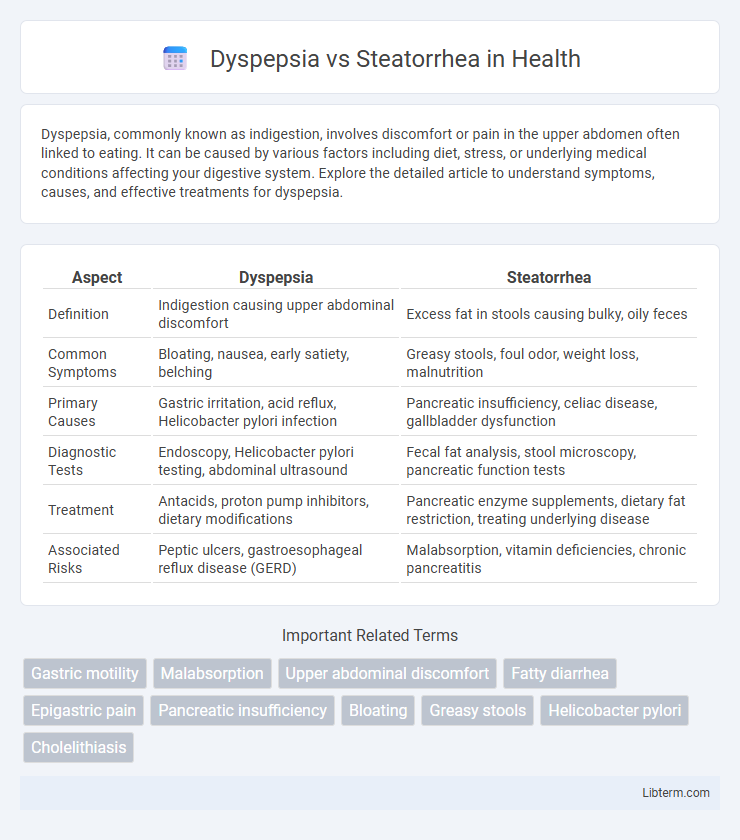
Dyspepsia, commonly known as indigestion, involves discomfort or pain in the upper abdomen often linked to eating. It can be caused by various factors including diet, stress, or underlying medical conditions affecting your digestive system. Explore the detailed article to understand symptoms, causes, and effective treatments for dyspepsia.
Table of Comparison
| Aspect | Dyspepsia | Steatorrhea |
|---|---|---|
| Definition | Indigestion causing upper abdominal discomfort | Excess fat in stools causing bulky, oily feces |
| Common Symptoms | Bloating, nausea, early satiety, belching | Greasy stools, foul odor, weight loss, malnutrition |
| Primary Causes | Gastric irritation, acid reflux, Helicobacter pylori infection | Pancreatic insufficiency, celiac disease, gallbladder dysfunction |
| Diagnostic Tests | Endoscopy, Helicobacter pylori testing, abdominal ultrasound | Fecal fat analysis, stool microscopy, pancreatic function tests |
| Treatment | Antacids, proton pump inhibitors, dietary modifications | Pancreatic enzyme supplements, dietary fat restriction, treating underlying disease |
| Associated Risks | Peptic ulcers, gastroesophageal reflux disease (GERD) | Malabsorption, vitamin deficiencies, chronic pancreatitis |
Understanding Dyspepsia: Definition and Symptoms
Dyspepsia, commonly known as indigestion, is characterized by persistent upper abdominal discomfort or pain, often accompanied by bloating, nausea, and early satiety. It differs significantly from steatorrhea, which involves the presence of excess fat in stool, indicating malabsorption issues. Recognizing symptoms like epigastric pain, belching, and heartburn is crucial for distinguishing dyspepsia from other gastrointestinal disorders.
Steatorrhea Explained: What It Is and Key Indicators
Steatorrhea is characterized by the presence of excess fat in stool, resulting in pale, bulky, and foul-smelling feces that float due to undigested fat. This condition often indicates malabsorption syndromes such as chronic pancreatitis, celiac disease, or cystic fibrosis, where the digestive system fails to properly absorb lipids. Key indicators include greasy stools, weight loss, abdominal cramping, and vitamin deficiencies from impaired fat absorption.
The Main Causes of Dyspepsia
Dyspepsia primarily arises from factors such as Helicobacter pylori infection, gastroesophageal reflux disease (GERD), and peptic ulcers, which disrupt the normal digestive process. Other significant causes include nonsteroidal anti-inflammatory drug (NSAID) use and functional dyspepsia with no identifiable organic disease. In contrast, steatorrhea results from malabsorption syndromes like chronic pancreatitis or celiac disease, characterized by fat maldigestion rather than the upper gastrointestinal discomfort seen in dyspepsia.
Common Triggers Behind Steatorrhea
Steatorrhea, characterized by excessive fat in stools, is commonly triggered by conditions that impair fat digestion or absorption, such as pancreatitis, celiac disease, and cystic fibrosis. Unlike dyspepsia, which involves upper abdominal discomfort often triggered by overeating, stress, or spicy foods, steatorrhea results primarily from malabsorption syndromes and pancreatic enzyme deficiencies. Identifying these underlying causes is essential for targeted treatment and symptom management.
Dyspepsia vs Steatorrhea: Symptom Comparison
Dyspepsia presents primarily with upper abdominal discomfort, bloating, nausea, and early satiety, indicating issues with digestion and gastric motility. In contrast, steatorrhea manifests through large, pale, foul-smelling stools with excessive fat content, reflecting malabsorption and pancreatic insufficiency. While dyspepsia focuses on discomfort and functional digestive symptoms, steatorrhea highlights a disruption in fat digestion and absorption.
Diagnosing Dyspepsia and Steatorrhea: Essential Tests
Diagnosing dyspepsia involves upper gastrointestinal endoscopy, Helicobacter pylori testing, and abdominal ultrasound to identify underlying causes such as gastritis or peptic ulcers. Steatorrhea diagnosis requires stool analysis for fat content, 72-hour fecal fat test, and pancreatic function tests including fecal elastase measurement to assess malabsorption or pancreatic insufficiency. Both conditions may necessitate blood tests for celiac disease antibodies and imaging studies like CT scan or MRI to evaluate structural abnormalities.
Risk Factors for Dyspepsia and Steatorrhea
Dyspepsia risk factors include Helicobacter pylori infection, nonsteroidal anti-inflammatory drug (NSAID) use, smoking, excessive alcohol consumption, and stress-related disorders. Steatorrhea risk factors often involve malabsorption syndromes such as celiac disease, chronic pancreatitis, cystic fibrosis, and bile acid deficiency. Both conditions can be influenced by dietary habits and underlying gastrointestinal disorders that impair digestion and absorption.
Treatment Options for Dyspepsia
Treatment options for dyspepsia include lifestyle modifications such as dietary changes and stress management, alongside pharmacological therapies like proton pump inhibitors (PPIs), H2 receptor antagonists, and antacids to reduce gastric acid secretion and alleviate symptoms. In cases where Helicobacter pylori infection is present, eradication therapy with antibiotics is essential for effective treatment. Unlike steatorrhea, which requires addressing malabsorption causes, dyspepsia management primarily focuses on symptom relief and acid suppression strategies.
Managing Steatorrhea: Effective Therapies
Managing steatorrhea requires addressing the underlying causes such as pancreatic insufficiency, celiac disease, or bile acid malabsorption. Pancreatic enzyme replacement therapy (PERT) is highly effective in improving fat digestion and reducing fatty stools in patients with pancreatic insufficiency. Dietary modifications, including low-fat intake and supplementation with medium-chain triglycerides (MCTs), alongside medications like bile acid binders, play a critical role in controlling symptoms and enhancing nutrient absorption.
Preventive Measures and Lifestyle Modifications
Dyspepsia prevention centers on dietary modifications such as avoiding spicy, fatty foods and reducing caffeine and alcohol intake to minimize gastric irritation. Steatorrhea management emphasizes a low-fat diet and supplementation of fat-soluble vitamins to improve fat absorption and reduce malabsorption symptoms. Both conditions benefit from stress reduction techniques and regular physical activity to enhance digestive function and overall gastrointestinal health.
Dyspepsia Infographic
 libterm.com
libterm.com