Cholecystitis is an inflammation of the gallbladder often caused by gallstones blocking the cystic duct, leading to severe abdominal pain and digestive issues. Hepatitis refers to inflammation of the liver, commonly resulting from viral infections, excessive alcohol use, or autoimmune diseases, and can cause symptoms like jaundice, fatigue, and abdominal discomfort. Explore the rest of this article to understand the differences, causes, and treatments for these two critical conditions affecting your digestive health.
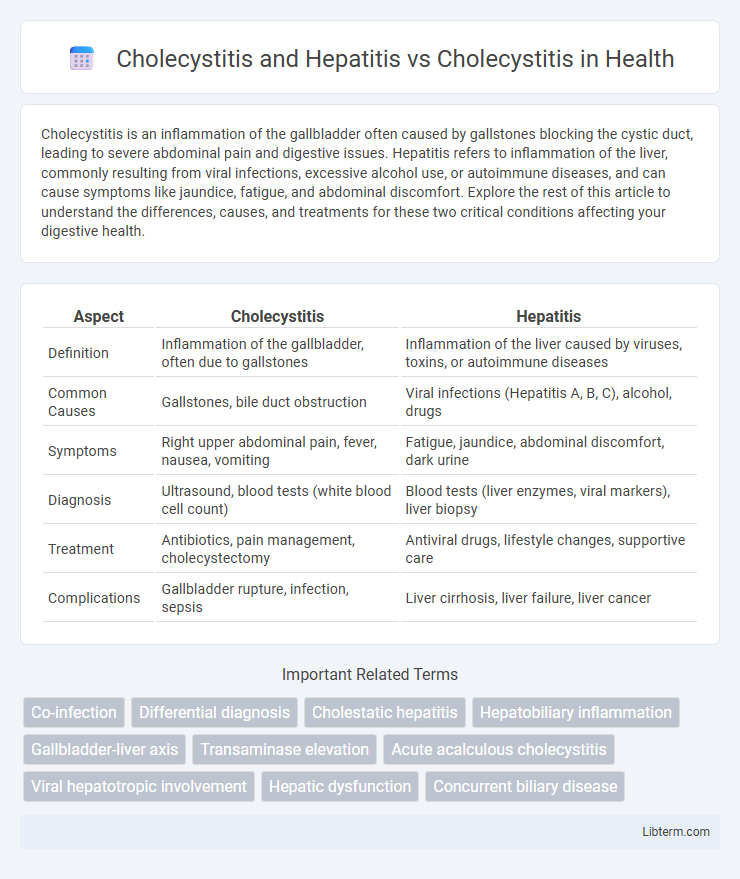
Table of Comparison
| Aspect | Cholecystitis | Hepatitis |
|---|---|---|
| Definition | Inflammation of the gallbladder, often due to gallstones | Inflammation of the liver caused by viruses, toxins, or autoimmune diseases |
| Common Causes | Gallstones, bile duct obstruction | Viral infections (Hepatitis A, B, C), alcohol, drugs |
| Symptoms | Right upper abdominal pain, fever, nausea, vomiting | Fatigue, jaundice, abdominal discomfort, dark urine |
| Diagnosis | Ultrasound, blood tests (white blood cell count) | Blood tests (liver enzymes, viral markers), liver biopsy |
| Treatment | Antibiotics, pain management, cholecystectomy | Antiviral drugs, lifestyle changes, supportive care |
| Complications | Gallbladder rupture, infection, sepsis | Liver cirrhosis, liver failure, liver cancer |
Overview of Cholecystitis
Cholecystitis is the inflammation of the gallbladder, typically caused by gallstones obstructing the cystic duct, leading to severe abdominal pain, fever, and nausea. Hepatitis primarily affects the liver, involving inflammation due to viral infections or toxins, which contrasts with the localized gallbladder inflammation seen in cholecystitis. Diagnosis of cholecystitis relies on imaging techniques like ultrasound and lab tests showing elevated white blood cells, distinguishing it from hepatitis that requires liver function tests and viral markers.
Understanding Hepatitis
Hepatitis is an inflammatory condition of the liver primarily caused by viral infections (hepatitis A, B, C, D, and E), autoimmune diseases, or toxic exposure such as alcohol or medications. Unlike cholecystitis, which involves inflammation of the gallbladder often due to gallstones blocking the cystic duct, hepatitis affects liver function and can lead to complications like liver fibrosis, cirrhosis, or hepatic failure. Understanding hepatitis requires recognizing its systemic symptoms such as jaundice, fatigue, and elevated liver enzymes (ALT, AST), which distinguish it from cholecystitis-specific signs like right upper quadrant pain and fever.
Key Differences: Cholecystitis vs Cholecystitis with Hepatitis
Cholecystitis primarily involves inflammation of the gallbladder, typically due to gallstones or infection, leading to localized symptoms like right upper quadrant pain and fever. When combined with hepatitis, inflammation extends to the liver, causing systemic symptoms such as jaundice, elevated liver enzymes, and generalized malaise. The key difference lies in the involvement of the liver in cholecystitis with hepatitis, resulting in more complex diagnostic and treatment considerations compared to isolated cholecystitis.
Pathophysiology Comparison
Cholecystitis involves inflammation of the gallbladder wall, usually triggered by gallstones obstructing the cystic duct, leading to bile stasis, mucosal injury, and secondary bacterial infection. Hepatitis, primarily viral or autoimmune in origin, causes inflammation of hepatocytes, disrupting liver function and impairing bile production and metabolism. While cholecystitis pathology centers on gallbladder obstruction and localized inflammation, hepatitis represents widespread hepatic cellular injury affecting systemic bile processing.
Clinical Manifestations and Symptoms
Cholecystitis primarily presents with right upper quadrant abdominal pain, fever, and nausea, often accompanied by a positive Murphy's sign, indicating gallbladder inflammation. Hepatitis, whether viral or alcoholic, typically manifests with systemic symptoms such as jaundice, fatigue, dark urine, and elevated liver enzymes (ALT and AST), reflecting liver inflammation. When cholecystitis coexists with hepatitis, patients may exhibit overlapping symptoms including abdominal pain and jaundice, complicating differential diagnosis and requiring careful evaluation of liver function tests and imaging studies.
Diagnostic Approaches
Diagnostic approaches for cholecystitis involve abdominal ultrasound to detect gallbladder inflammation and Murphy's sign for clinical assessment, while hepatitis diagnosis primarily relies on serological tests for viral markers and liver function tests indicating hepatic injury. In cases of cholecystitis combined with hepatitis, differentiation requires both imaging studies and detailed liver panels to evaluate concurrent gallbladder inflammation and hepatic dysfunction. Early diagnosis utilizes abdominal ultrasound, liver enzyme profiles, and specific viral antigen or antibody screenings to guide targeted treatment strategies.
Imaging and Laboratory Findings
Cholecystitis typically presents with gallbladder wall thickening and pericholecystic fluid on ultrasound, elevated white blood cell count, and increased C-reactive protein levels. Hepatitis primarily shows liver inflammation on imaging such as hepatomegaly or hypoechoic areas on ultrasound, alongside markedly elevated aminotransferases (ALT and AST) and bilirubin levels in laboratory tests. Coexisting cholecystitis and hepatitis complicate diagnosis by overlapping imaging signs and mixed elevation of inflammatory markers and liver enzymes.
Treatment Strategies
Cholecystitis treatment primarily involves antibiotics and potential gallbladder removal through cholecystectomy, targeting inflammation caused by gallstones or infection. Hepatitis management depends on the viral or autoimmune etiology, utilizing antiviral medications or immunosuppressants, which differ significantly from cholecystitis therapies. Overlapping cases require careful differential diagnosis to optimize treatment plans, avoiding unnecessary surgical interventions when liver inflammation predominates.
Prognosis and Complications
Cholecystitis combined with hepatitis presents a more complex prognosis due to liver inflammation impairing bile flow and immune response, increasing risk of severe complications such as sepsis, liver failure, and bile duct obstruction. Isolated cholecystitis generally has a favorable prognosis when treated promptly, but delayed management can lead to gallbladder rupture, abscess formation, and peritonitis. Monitoring liver function tests and early intervention are critical in patients with concurrent hepatitis to reduce morbidity and improve overall outcomes.
Prevention and Patient Education
Effective prevention of cholecystitis involves maintaining a healthy diet low in fatty foods and managing risk factors like obesity and gallstones, while hepatitis prevention focuses on vaccination, safe needle practices, and avoiding contaminated food or water. Patient education should emphasize the importance of early symptom recognition, such as abdominal pain and jaundice, and adherence to medical advice to prevent complications in both conditions. Promoting lifestyle modifications and timely medical consultation can reduce the incidence and severity of cholecystitis and hepatitis.
Cholecystitis and Hepatitis Infographic
 libterm.com
libterm.com