Thrombocythemia and Essential Thrombocytosis are disorders characterized by an abnormally high platelet count, increasing the risk of blood clots, strokes, and bleeding complications. Understanding the causes, symptoms, and treatment options is crucial for managing these conditions effectively. Explore the full article to learn how you can recognize symptoms and find the best strategies for treatment.
Table of Comparison
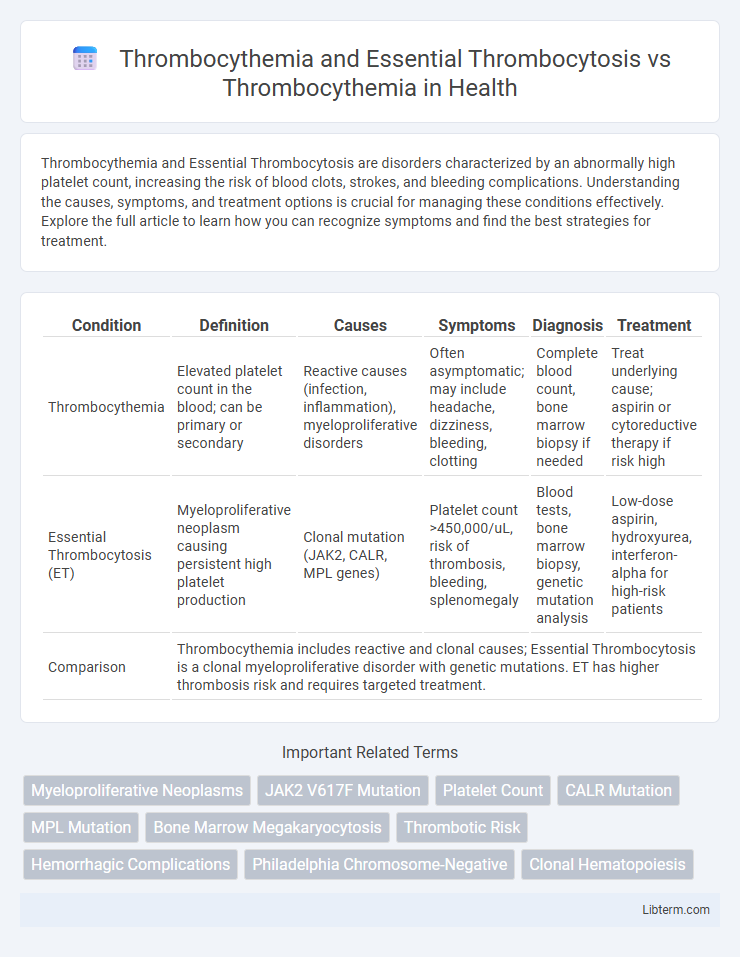
| Condition | Definition | Causes | Symptoms | Diagnosis | Treatment |
|---|---|---|---|---|---|
| Thrombocythemia | Elevated platelet count in the blood; can be primary or secondary | Reactive causes (infection, inflammation), myeloproliferative disorders | Often asymptomatic; may include headache, dizziness, bleeding, clotting | Complete blood count, bone marrow biopsy if needed | Treat underlying cause; aspirin or cytoreductive therapy if risk high |
| Essential Thrombocytosis (ET) | Myeloproliferative neoplasm causing persistent high platelet production | Clonal mutation (JAK2, CALR, MPL genes) | Platelet count >450,000/uL, risk of thrombosis, bleeding, splenomegaly | Blood tests, bone marrow biopsy, genetic mutation analysis | Low-dose aspirin, hydroxyurea, interferon-alpha for high-risk patients |
| Comparison | Thrombocythemia includes reactive and clonal causes; Essential Thrombocytosis is a clonal myeloproliferative disorder with genetic mutations. ET has higher thrombosis risk and requires targeted treatment. | ||||
Understanding Thrombocythemia: Definition and Overview
Thrombocythemia, also known as thrombocytosis, is a hematological condition characterized by an elevated platelet count in the blood exceeding 450,000 platelets per microliter. Essential Thrombocythemia (ET) is a specific type of primary thrombocythemia caused by clonal proliferation of megakaryocytes in the bone marrow, leading to excessive platelet production without a reactive cause. Differentiating ET from secondary (reactive) thrombocythemia involves ruling out underlying conditions such as inflammation, infection, or iron deficiency that may cause transient platelet elevation.
Essential Thrombocytosis: Causes and Pathogenesis
Essential Thrombocytosis (ET) is a myeloproliferative neoplasm characterized by the clonal proliferation of megakaryocytes in the bone marrow, leading to persistent thrombocytosis. Key genetic mutations in JAK2, CALR, and MPL genes drive aberrant signaling pathways that promote uncontrolled platelet production and contribute to thrombotic complications. Unlike reactive thrombocythemia, which results from secondary causes such as inflammation or iron deficiency, ET arises primarily from intrinsic hematopoietic stem cell abnormalities affecting cellular proliferation and differentiation.
Thrombocythemia vs. Thrombocytosis: Key Differences
Thrombocythemia and essential thrombocytosis both describe conditions of elevated platelet counts, but essential thrombocytosis is a type of primary thrombocythemia characterized by clonal bone marrow stem cell proliferation. Reactive thrombocythemia, or secondary thrombocythemia, results from external factors such as inflammation or infection, distinguishing it from essential thrombocytosis's genetic basis. Key differences include the origin of the platelet increase--clonal in essential thrombocytosis versus reactive in thrombocythemia--and associated risks like thrombosis, which are higher in essential thrombocytosis.
Clinical Presentation of Essential Thrombocytosis
Essential Thrombocytosis (ET) primarily presents with elevated platelet counts often exceeding 450,000/uL, leading to symptoms such as microvascular disturbances including headaches, dizziness, erythromelalgia, and digital ischemia. Patients may experience thrombotic complications involving both arterial and venous systems, as well as hemorrhagic events due to dysfunctional platelets. Unlike secondary thrombocythemia, which is reactive and transient, ET is a chronic myeloproliferative neoplasm characterized by clonal platelet proliferation and presence of mutations in JAK2, CALR, or MPL genes.
Diagnostic Criteria for Thrombocythemia
Thrombocythemia diagnosis is primarily based on sustained platelet counts above 450,000 per microliter, confirmed through repeated blood tests and bone marrow biopsy revealing increased megakaryocyte proliferation. Essential thrombocytosis, a subtype of thrombocythemia, is distinguished by the presence of JAK2, CALR, or MPL gene mutations combined with exclusion of reactive causes such as infection or iron deficiency. Diagnostic criteria emphasize ruling out secondary thrombocytosis by thorough clinical evaluation and laboratory testing for clonal markers and bone marrow morphology.
Laboratory Findings: Platelet Count and Blood Markers
Essential thrombocytosis and thrombocythemia both present with elevated platelet counts, often exceeding 450,000 per microliter, but essential thrombocytosis typically shows sustained thrombocytosis with clonal proliferation markers such as JAK2, CALR, or MPL mutations. Laboratory findings in thrombocythemia reveal high platelet counts without these mutations, indicating reactive or secondary causes. Blood markers like erythropoietin levels and molecular studies help differentiate essential thrombocytosis, characterized by increased megakaryocyte proliferation, from reactive thrombocythemia caused by inflammation or iron deficiency.
Risk Factors and Associated Conditions
Thrombocythemia, including Essential Thrombocytosis (ET), is characterized by an elevated platelet count often linked to JAK2, CALR, or MPL gene mutations that increase thrombotic risk. Risk factors such as advanced age, history of thrombosis, cardiovascular disease, and the presence of acquired von Willebrand disease significantly influence disease complications. Associated conditions include myeloproliferative neoplasms, splenomegaly, hemorrhage, and increased susceptibility to stroke or deep vein thrombosis.
Complications: Thrombosis and Bleeding Risks
Essential thrombocytosis, a subset of thrombocythemia, presents a heightened risk of thrombosis due to abnormal platelet function and proliferation, leading to complications such as stroke, myocardial infarction, and deep vein thrombosis. Both conditions may also cause bleeding events, particularly when platelet counts are extremely elevated or dysfunctional, resulting in impaired clot formation. Effective management requires balancing these dual risks to reduce thrombotic events while minimizing hemorrhagic complications.
Current Treatment Approaches for Essential Thrombocytosis
Essential thrombocytosis (ET), a myeloproliferative neoplasm characterized by elevated platelet counts, is primarily managed by risk stratification and cytoreductive therapies such as hydroxyurea and interferon-alpha. Aspirin is frequently prescribed to reduce thrombotic events, especially in patients with cardiovascular risk factors, while anagrelide may be used to control platelet levels when hydroxyurea is contraindicated. Recent advances include targeting JAK2 mutations with inhibitors like ruxolitinib, improving outcomes for patients resistant or intolerant to first-line therapies.
Prognosis and Long-term Management Strategies
Thrombocythemia, particularly Essential Thrombocytosis (ET), presents a generally favorable prognosis with proper management, though risks of thrombotic events require vigilant monitoring. Long-term management strategies for ET focus on risk stratification involving age, history of thrombosis, and platelet count, often incorporating low-dose aspirin and cytoreductive therapy such as hydroxyurea to prevent complications. In contrast, secondary thrombocythemia typically resolves with treatment of the underlying cause, exhibiting a less complex prognosis and minimal long-term management needs.
Thrombocythemia and Essential Thrombocytosis Infographic
 libterm.com
libterm.com