A thrombus is a blood clot that forms within a blood vessel, potentially obstructing normal blood flow and leading to serious health complications such as stroke or heart attack. Understanding the causes, symptoms, and treatments of thrombus is crucial for early detection and prevention. Explore the rest of this article to learn more about how a thrombus can affect your health and the steps you can take to manage it effectively.
Table of Comparison
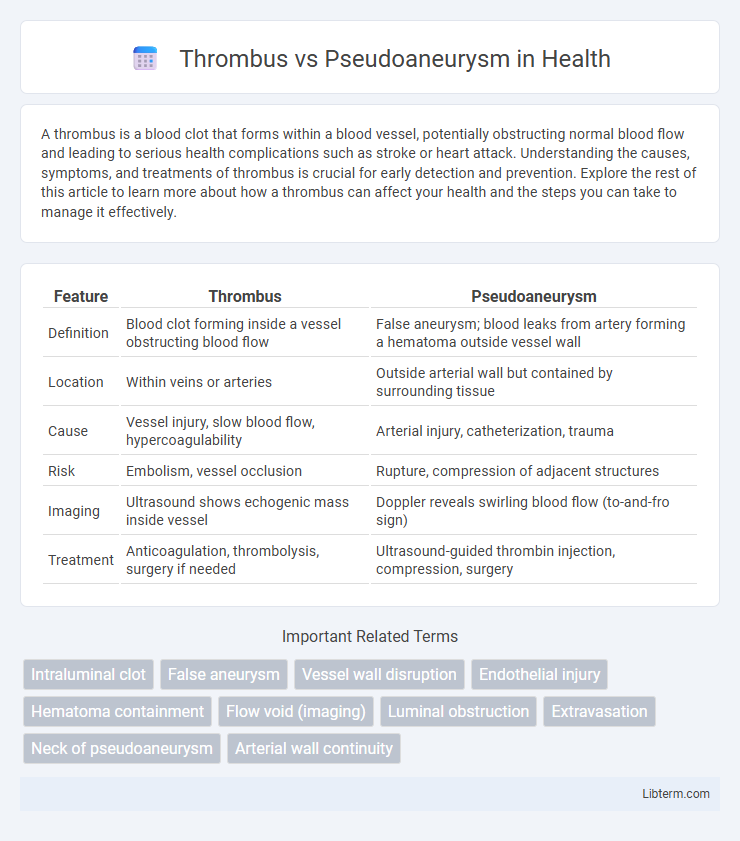
| Feature | Thrombus | Pseudoaneurysm |
|---|---|---|
| Definition | Blood clot forming inside a vessel obstructing blood flow | False aneurysm; blood leaks from artery forming a hematoma outside vessel wall |
| Location | Within veins or arteries | Outside arterial wall but contained by surrounding tissue |
| Cause | Vessel injury, slow blood flow, hypercoagulability | Arterial injury, catheterization, trauma |
| Risk | Embolism, vessel occlusion | Rupture, compression of adjacent structures |
| Imaging | Ultrasound shows echogenic mass inside vessel | Doppler reveals swirling blood flow (to-and-fro sign) |
| Treatment | Anticoagulation, thrombolysis, surgery if needed | Ultrasound-guided thrombin injection, compression, surgery |
Introduction to Vascular Abnormalities
Thrombus and pseudoaneurysm represent distinct vascular abnormalities with critical clinical implications. A thrombus is a blood clot formed within a vessel, obstructing blood flow and potentially causing ischemia or embolism. Pseudoaneurysm, or false aneurysm, occurs when a blood vessel wall is injured, leading to a contained rupture and blood collection outside the vessel lumen, often detectable via ultrasound or angiography.
Defining Thrombus: Causes and Characteristics
A thrombus is a blood clot that forms within a blood vessel or the heart, primarily caused by endothelial injury, abnormal blood flow, or hypercoagulability conditions such as thrombophilia. Its characteristics include firm adherence to the vessel wall, potential to obstruct blood flow, and composition mainly of fibrin, platelets, and trapped blood cells. Unlike pseudoaneurysms, which are false aneurysms involving vessel wall rupture and blood leakage, thrombi represent localized coagulation without vessel wall disruption.
Understanding Pseudoaneurysm: Formation and Risk Factors
Pseudoaneurysm forms when a blood vessel wall is injured, causing blood to leak and collect between the vessel layers or surrounding tissue, creating a sac-like structure. Common risk factors include trauma, catheterization procedures, infections, and connective tissue disorders that weaken vessel integrity. Unlike a thrombus, which is a blood clot within a vessel, a pseudoaneurysm involves an actual breach in the vessel wall leading to a contained hematoma.
Key Differences Between Thrombus and Pseudoaneurysm
A thrombus is a blood clot that forms within a blood vessel, obstructing blood flow, whereas a pseudoaneurysm is a contained rupture of a blood vessel wall causing a blood-filled cavity communicating with the artery. Thrombi are composed of fibrin, platelets, and red blood cells adhering to the vessel wall, while pseudoaneurysms result from vessel wall injury and blood leakage confined by surrounding tissues. Diagnostic imaging such as ultrasound or angiography helps differentiate thrombus, which appears as an intraluminal echogenic mass, from pseudoaneurysm, which shows a characteristic swirling blood flow pattern known as the "yin-yang" sign.
Clinical Presentation: Signs and Symptoms Comparison
Thrombus typically presents with localized pain, swelling, and possible limb ischemia due to vessel occlusion, often accompanied by erythema and warmth in the affected area. In contrast, a pseudoaneurysm often manifests as a pulsatile mass with a palpable thrill, bruising, and sometimes audible bruit, reflecting turbulent blood flow outside the arterial lumen. Both conditions may cause tenderness, but pseudoaneurysms are more likely to produce neurological symptoms if compressing nearby nerves, whereas thrombi commonly lead to distal vascular compromise.
Diagnostic Approaches: Imaging and Laboratory Tests
Diagnostic approaches for thrombus primarily involve Doppler ultrasound to detect blood flow obstruction and CT or MRI angiography for detailed vessel visualization. Pseudoaneurysm diagnosis relies heavily on color Doppler ultrasound, which reveals the characteristic "yin-yang" blood flow pattern, while contrast-enhanced CT provides precise anatomical definition. Laboratory tests, such as D-dimer levels, may aid thrombus detection but have limited utility in identifying pseudoaneurysms, emphasizing imaging as the cornerstone of differential diagnosis.
Management Strategies for Thrombus
Management strategies for thrombus primarily involve anticoagulation therapy to prevent clot propagation and reduce the risk of embolism, with agents such as heparin and warfarin commonly used. In cases where anticoagulation is contraindicated or ineffective, mechanical thrombectomy or thrombolytic therapy with tissue plasminogen activator may be indicated. Close monitoring through imaging modalities like ultrasound or CT angiography is essential to assess thrombus resolution and guide therapeutic adjustments.
Treatment Options for Pseudoaneurysm
Treatment options for pseudoaneurysm primarily include ultrasound-guided thrombin injection, which promotes clotting within the pseudoaneurysm sac, leading to its resolution. Surgical repair or endovascular techniques such as coil embolization may be necessary for large, expanding, or symptomatic pseudoaneurysms not amenable to minimally invasive methods. Compression therapy using ultrasound guidance is an alternative for small, uncomplicated pseudoaneurysms, offering a noninvasive approach to promote thrombosis and vessel wall healing.
Complications and Prognosis
Thrombus formation can lead to complications such as embolism, stroke, and infarction due to vessel obstruction, often requiring anticoagulant therapy for prognosis improvement. Pseudoaneurysms risk rupture and hemorrhage, which may result in life-threatening bleeding and necessitate surgical intervention or endovascular repair for favorable outcomes. Prognosis of thrombus depends on timely management of underlying causes, whereas pseudoaneurysm prognosis hinges on size, location, and promptness of treatment.
Prevention and Patient Education
Preventing thrombus formation involves maintaining adequate hydration, regular physical activity, and adherence to prescribed anticoagulant therapy to reduce blood clot risks. Educating patients about recognizing early symptoms of pseudoaneurysm, such as localized swelling and pain near vascular access sites, is critical for timely medical intervention. Emphasizing proper wound care and avoiding trauma to catheter sites helps minimize complications related to pseudoaneurysms.
Thrombus Infographic
 libterm.com
libterm.com