Gastroparesis is a condition where your stomach muscles don't function properly, leading to delayed emptying of stomach contents. Symptoms often include nausea, vomiting, bloating, and abdominal pain, significantly affecting digestion and quality of life. Discover effective treatments and management strategies in the rest of this article to better control your symptoms.
Table of Comparison
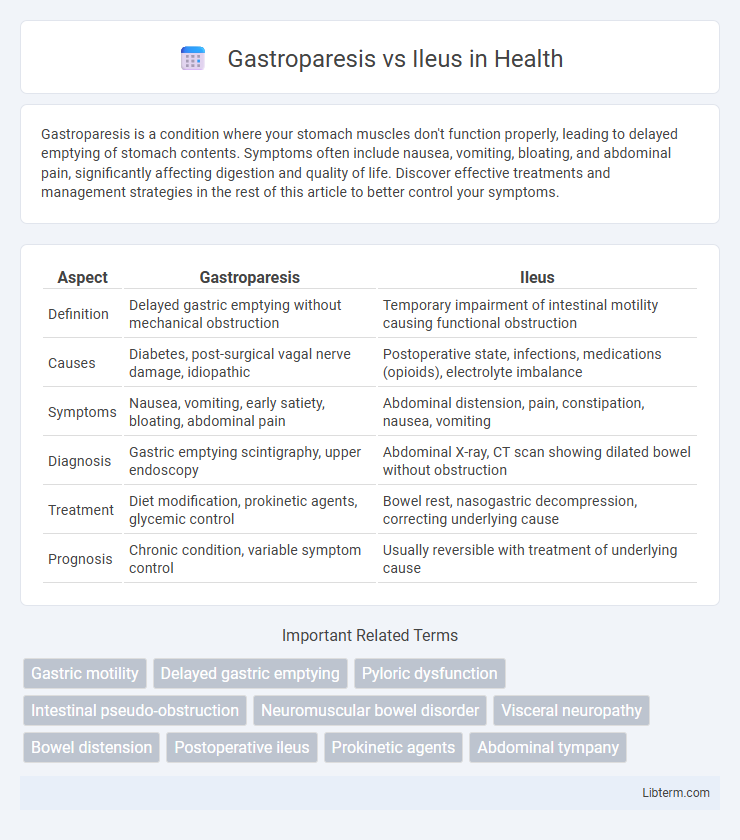
| Aspect | Gastroparesis | Ileus |
|---|---|---|
| Definition | Delayed gastric emptying without mechanical obstruction | Temporary impairment of intestinal motility causing functional obstruction |
| Causes | Diabetes, post-surgical vagal nerve damage, idiopathic | Postoperative state, infections, medications (opioids), electrolyte imbalance |
| Symptoms | Nausea, vomiting, early satiety, bloating, abdominal pain | Abdominal distension, pain, constipation, nausea, vomiting |
| Diagnosis | Gastric emptying scintigraphy, upper endoscopy | Abdominal X-ray, CT scan showing dilated bowel without obstruction |
| Treatment | Diet modification, prokinetic agents, glycemic control | Bowel rest, nasogastric decompression, correcting underlying cause |
| Prognosis | Chronic condition, variable symptom control | Usually reversible with treatment of underlying cause |
Understanding Gastroparesis and Ileus: Key Differences
Gastroparesis is a chronic disorder characterized by delayed gastric emptying without mechanical obstruction, while ileus refers to a temporary cessation of intestinal motility often caused by surgery or infection. Gastroparesis primarily affects stomach motility due to nerve damage, commonly seen in diabetic patients, whereas ileus involves functional paralysis of the intestines, leading to bowel obstruction symptoms. Differentiating these conditions relies on diagnostic methods like gastric emptying studies for gastroparesis and abdominal imaging for ileus to guide appropriate treatment strategies.
Causes of Gastroparesis vs Ileus
Gastroparesis primarily results from nerve damage, especially to the vagus nerve, often caused by diabetes, viral infections, or certain medications. Ileus is typically triggered by factors such as abdominal surgery, infections, electrolyte imbalances, or medications that slow intestinal motility. While gastroparesis involves delayed gastric emptying without mechanical obstruction, ileus is characterized by temporary paralysis of intestinal muscles.
Clinical Symptoms Comparison
Gastroparesis presents with symptoms such as persistent nausea, early satiety, bloating, and intermittent vomiting due to delayed gastric emptying, often without mechanical obstruction. Ileus is characterized by diffuse abdominal pain, distension, absent bowel sounds, and constipation caused by a temporary impairment of intestinal motility. Unlike gastroparesis, ileus typically results in more generalized gastrointestinal dysfunction affecting both small and large intestines.
Diagnostic Approaches for Gastroparesis and Ileus
Gastroparesis diagnosis primarily involves gastric emptying scintigraphy, which measures the rate at which food leaves the stomach, alongside electrogastrography to assess gastric motility patterns. Ileus diagnosis relies on abdominal X-rays and CT scans to identify bowel dilation and absence of mechanical obstruction, complemented by clinical assessment of bowel sounds and patient symptoms. Both conditions benefit from thorough patient history and physical examination to distinguish between functional motility delay in gastroparesis and paralysis of intestinal muscles in ileus.
Risk Factors and Predisposing Conditions
Gastroparesis is commonly associated with diabetes mellitus, particularly type 1 and type 2, due to autonomic neuropathy affecting gastric motility, while ileus frequently occurs after abdominal surgery, especially following procedures involving the intestines or colorectal region. Other predisposing conditions for gastroparesis include viral infections, Parkinson's disease, and connective tissue disorders, whereas risk factors for ileus encompass electrolyte imbalances, opioid use, and peritonitis. Chronic conditions such as hypothyroidism and systemic sclerosis may also increase susceptibility to gastroparesis, contrasting with ileus, which is often triggered by acute insults to the gastrointestinal tract.
Pathophysiology: How Gastroparesis Differs from Ileus
Gastroparesis is characterized by delayed gastric emptying due to impaired vagal nerve function or smooth muscle dysfunction, leading to disrupted coordination of gastric motility without mechanical obstruction. Ileus involves a temporary cessation of intestinal peristalsis caused by factors such as intestinal inflammation, electrolyte imbalances, or postoperative neural reflexes affecting both small and large bowel motility. Unlike ileus, which affects the entire bowel, gastroparesis primarily impairs gastric emptying, reflecting distinct pathophysiological mechanisms within the enteric nervous system.
Treatment Strategies: Gastroparesis vs Ileus
Treatment strategies for gastroparesis primarily involve dietary modifications such as small, frequent meals low in fat and fiber, prokinetic medications like metoclopramide or erythromycin to enhance gastric motility, and in severe cases, interventions including gastric electrical stimulation or jejunal feeding tubes. Ileus treatment focuses on bowel rest, often requiring nasogastric decompression to relieve obstruction, correction of underlying causes such as electrolyte imbalances or medication effects, and gradual reintroduction of diet once bowel function resumes. While gastroparesis management targets enhancing delayed gastric emptying, ileus treatment emphasizes resolution of bowel paralysis and promoting return of normal intestinal motility.
Complications and Prognosis
Gastroparesis complications include malnutrition, dehydration, and bezoar formation due to delayed gastric emptying, with prognosis varying based on underlying causes and severity. Ileus often leads to bowel obstruction, electrolyte imbalances, and risk of bowel ischemia, with prognosis dependent on timely medical intervention and resolution of the underlying cause. Both conditions can cause significant morbidity but differ in their pathophysiology and treatment outcomes.
Dietary and Lifestyle Management
Dietary and lifestyle management for gastroparesis includes consuming small, frequent meals low in fat and fiber to enhance gastric emptying and prevent symptoms like nausea and bloating. In contrast, ileus management emphasizes bowel rest with minimal oral intake initially, gradually reintroducing a low-residue diet to reduce intestinal workload and stimulate motility. Both conditions benefit from hydration, avoiding heavy meals, and tailored nutritional support to optimize gastrointestinal function and recovery.
When to Seek Medical Attention
Gastroparesis requires medical attention when symptoms such as persistent nausea, vomiting, or severe abdominal pain interfere with nutrition or hydration, or if there are signs of dehydration or weight loss. Ileus demands urgent care if there is inability to pass gas or stool, severe abdominal distension, or sudden worsening of pain, as it may indicate bowel obstruction or ischemia. Prompt evaluation with imaging and laboratory tests is essential to prevent complications in both conditions.
Gastroparesis Infographic
 libterm.com
libterm.com