Rheumatoid arthritis is a chronic autoimmune condition causing inflammation, pain, and joint damage, primarily affecting the hands and feet. Early diagnosis and targeted treatments can help manage symptoms and improve your quality of life. Explore the rest of this article to understand effective strategies for living with rheumatoid arthritis.
Table of Comparison
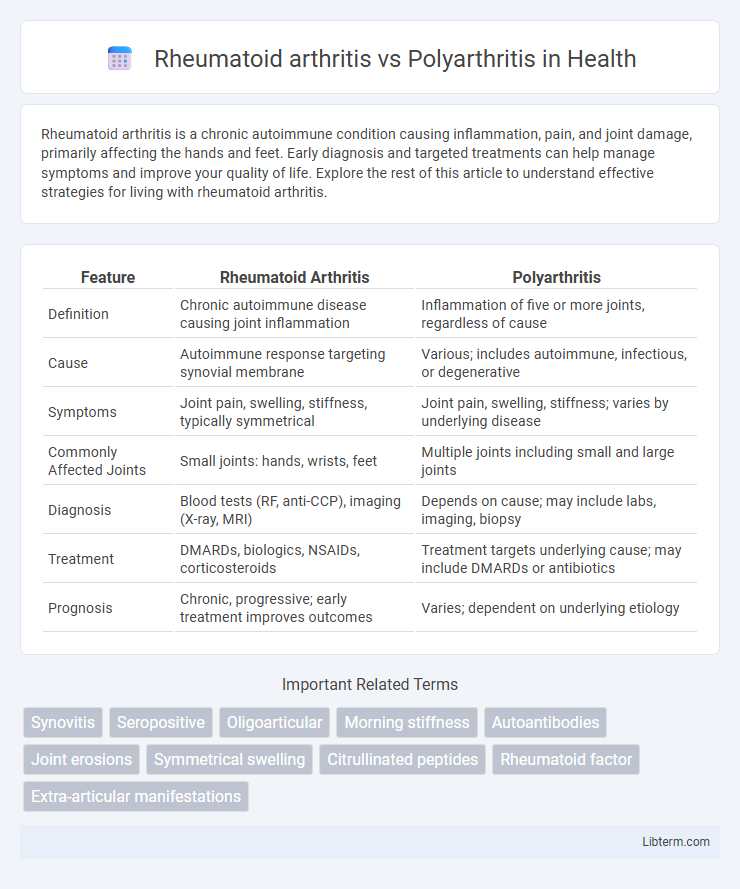
| Feature | Rheumatoid Arthritis | Polyarthritis |
|---|---|---|
| Definition | Chronic autoimmune disease causing joint inflammation | Inflammation of five or more joints, regardless of cause |
| Cause | Autoimmune response targeting synovial membrane | Various; includes autoimmune, infectious, or degenerative |
| Symptoms | Joint pain, swelling, stiffness, typically symmetrical | Joint pain, swelling, stiffness; varies by underlying disease |
| Commonly Affected Joints | Small joints: hands, wrists, feet | Multiple joints including small and large joints |
| Diagnosis | Blood tests (RF, anti-CCP), imaging (X-ray, MRI) | Depends on cause; may include labs, imaging, biopsy |
| Treatment | DMARDs, biologics, NSAIDs, corticosteroids | Treatment targets underlying cause; may include DMARDs or antibiotics |
| Prognosis | Chronic, progressive; early treatment improves outcomes | Varies; dependent on underlying etiology |
Overview of Rheumatoid Arthritis and Polyarthritis
Rheumatoid arthritis (RA) is a chronic autoimmune disorder primarily affecting synovial joints, characterized by persistent inflammation, joint pain, swelling, and progressive joint damage. Polyarthritis refers to the simultaneous inflammation of five or more joints, which can result from various conditions, including rheumatoid arthritis, viral infections, or other autoimmune diseases. RA is a leading cause of polyarthritis, distinguished by symmetrical joint involvement, presence of rheumatoid factor (RF), anti-cyclic citrullinated peptide (anti-CCP) antibodies, and systemic manifestations such as fatigue and morning stiffness.
Defining Rheumatoid Arthritis
Rheumatoid arthritis is a chronic autoimmune disorder characterized by inflammation primarily affecting the synovial joints, leading to pain, swelling, and eventual joint deformity. Unlike polyarthritis, which simply refers to inflammation in multiple joints without specifying cause or pathogenesis, rheumatoid arthritis involves a specific immune response targeting joint tissues. Early diagnosis and treatment of rheumatoid arthritis are crucial to prevent irreversible joint damage and improve long-term functional outcomes.
Understanding Polyarthritis
Polyarthritis refers to the inflammation of five or more joints simultaneously, often causing widespread pain and stiffness, and can be a symptom of various underlying conditions, including rheumatoid arthritis. Unlike rheumatoid arthritis, which is a specific autoimmune disorder characterized by symmetrical joint involvement and systemic inflammation, polyarthritis is a broader clinical manifestation that may result from infections, autoimmune diseases, or other inflammatory processes. Accurate diagnosis and treatment depend on identifying the specific cause of polyarthritis through clinical evaluation, laboratory tests, and imaging studies, as effective management varies accordingly.
Key Differences Between Rheumatoid Arthritis and Polyarthritis
Rheumatoid arthritis is a chronic autoimmune disorder primarily affecting symmetrical joints and causing inflammation, pain, and eventual joint deformity, whereas polyarthritis simply describes inflammation in five or more joints regardless of cause. Rheumatoid arthritis often involves specific biomarkers such as rheumatoid factor (RF) and anti-cyclic citrullinated peptide (anti-CCP) antibodies, which are typically absent in other forms of polyarthritis caused by infections or other diseases. The key clinical difference lies in the chronic, systemic nature and autoimmune etiology of rheumatoid arthritis compared to the broader, non-specific definition of polyarthritis.
Causes and Risk Factors
Rheumatoid arthritis is primarily caused by an autoimmune response where the immune system attacks joint lining, with genetic predisposition and environmental triggers like smoking increasing risk. Polyarthritis refers to inflammation affecting five or more joints, often linked to diverse conditions such as infections, autoimmune diseases like rheumatoid arthritis, and metabolic disorders. Risk factors for polyarthritis vary widely depending on the underlying cause but frequently include autoimmune susceptibility, age, and exposure to infectious agents.
Clinical Symptoms and Presentation
Rheumatoid arthritis (RA) primarily presents with symmetrical joint pain, swelling, and morning stiffness lasting over an hour, commonly affecting small joints such as the metacarpophalangeal and proximal interphalangeal joints. Polyarthritis refers to inflammation involving five or more joints and can occur in various diseases, but when caused by RA, it displays persistent synovitis with systemic symptoms like fatigue and low-grade fever. Joint deformities, rheumatoid nodules, and elevated inflammatory markers like ESR and CRP are characteristic of RA's clinical presentation compared to other causes of polyarthritis.
Diagnostic Criteria and Procedures
Rheumatoid arthritis (RA) diagnosis involves specific criteria such as the 2010 ACR/EULAR classification, emphasizing joint involvement, serology (RF and anti-CCP antibodies), acute-phase reactants, and symptom duration. Polyarthritis, characterized by inflammation in five or more joints, requires differential diagnosis using clinical examination, imaging like ultrasound or MRI, and lab tests to distinguish from RA and other causes like psoriatic arthritis or lupus. Diagnostic procedures prioritize blood markers, joint fluid analysis, and radiographic evidence to accurately identify the underlying inflammatory arthritis type.
Treatment Approaches
Rheumatoid arthritis treatment primarily involves disease-modifying antirheumatic drugs (DMARDs) such as methotrexate, biologics like TNF inhibitors, and corticosteroids to reduce inflammation and prevent joint damage. In contrast, polyarthritis treatment varies based on the underlying cause but often includes nonsteroidal anti-inflammatory drugs (NSAIDs), corticosteroids, and physiotherapy to manage symptoms and maintain joint function. Both conditions may require individualized treatment plans emphasizing early intervention and regular monitoring to improve patient outcomes.
Prognosis and Complications
Rheumatoid arthritis (RA) often leads to progressive joint damage and deformities, with a variable prognosis influenced by early diagnosis and aggressive treatment; complications include cardiovascular disease, lung involvement, and osteoporosis. Polyarthritis, defined by inflammation of five or more joints, may result from various underlying conditions, with prognosis and complications depending on the specific etiology, such as infection, autoimmune disease, or crystal arthropathies. Early management in both conditions is crucial to prevent joint destruction and systemic complications, improving long-term functional outcomes.
When to Seek Medical Advice
Persistent joint pain, swelling, and stiffness lasting more than six weeks warrant prompt medical evaluation to differentiate rheumatoid arthritis from polyarthritis. Early diagnosis through clinical examination, blood tests for rheumatoid factor and anti-CCP antibodies, and imaging studies is crucial to prevent joint damage and optimize treatment. Seek immediate medical advice if symptoms worsen rapidly or if systemic signs like fever, weight loss, or fatigue accompany joint problems.
Rheumatoid arthritis Infographic
 libterm.com
libterm.com