Alveolar refers to the small air sacs in the lungs where gas exchange occurs between oxygen and carbon dioxide in the bloodstream. These structures are crucial for efficient breathing and oxygenating your body. Discover more about how alveolar function impacts your respiratory health in the rest of this article.
Table of Comparison
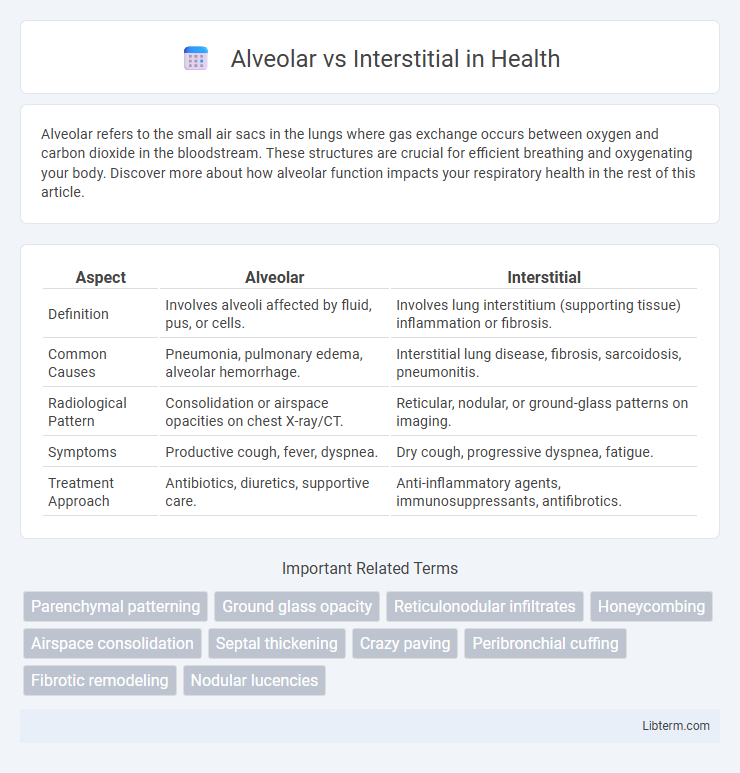
| Aspect | Alveolar | Interstitial |
|---|---|---|
| Definition | Involves alveoli affected by fluid, pus, or cells. | Involves lung interstitium (supporting tissue) inflammation or fibrosis. |
| Common Causes | Pneumonia, pulmonary edema, alveolar hemorrhage. | Interstitial lung disease, fibrosis, sarcoidosis, pneumonitis. |
| Radiological Pattern | Consolidation or airspace opacities on chest X-ray/CT. | Reticular, nodular, or ground-glass patterns on imaging. |
| Symptoms | Productive cough, fever, dyspnea. | Dry cough, progressive dyspnea, fatigue. |
| Treatment Approach | Antibiotics, diuretics, supportive care. | Anti-inflammatory agents, immunosuppressants, antifibrotics. |
Introduction to Alveolar and Interstitial Lung Diseases
Alveolar lung diseases primarily affect the alveoli, the tiny air sacs in the lungs where gas exchange occurs, leading to symptoms like shortness of breath and cough due to alveolar filling or collapse. Interstitial lung diseases involve inflammation and scarring of the lung interstitium, the tissue surrounding the alveoli, causing progressive stiffness and impaired oxygen diffusion. Both conditions disrupt normal lung function but differ in pathophysiology, radiographic patterns, and treatment approaches, making accurate diagnosis critical for effective management.
Anatomy of Alveoli vs Interstitium
The alveoli are tiny, balloon-like air sacs in the lungs where gas exchange occurs, lined with a thin epithelial layer and surrounded by capillaries. The interstitium is the connective tissue framework between alveoli, composed of fibroblasts, collagen, elastin fibers, and a network of capillaries, providing structural support and facilitating fluid balance. While alveoli enable oxygen and carbon dioxide diffusion, the interstitium maintains the lung's elasticity and integrity.
Key Differences Between Alveolar and Interstitial Disorders
Alveolar disorders primarily affect the air sacs (alveoli) within the lungs, leading to impaired gas exchange due to fluid, cells, or other substances filling the alveolar spaces, as seen in pulmonary edema or alveolar hemorrhage. Interstitial disorders involve the lung interstitium, the tissue surrounding the alveoli, causing fibrosis or inflammation that stiffens the lung and reduces its elasticity, exemplified by idiopathic pulmonary fibrosis or hypersensitivity pneumonitis. Key differences include the location of pathology--alveolar spaces versus interstitial tissue--and the resulting impact on lung function, with alveolar disorders typically causing consolidation and airspace filling, while interstitial disorders result in thickening and scarring of the lung parenchyma.
Common Causes of Alveolar Diseases
Common causes of alveolar diseases include pulmonary edema, pneumonia, alveolar hemorrhage, and acute respiratory distress syndrome (ARDS). These conditions primarily affect the air sacs (alveoli), leading to fluid accumulation, inflammation, and impaired gas exchange. Identifying specific causes such as bacterial or viral infections and cardiogenic or non-cardiogenic pulmonary edema is essential for targeted treatment.
Common Causes of Interstitial Diseases
Common causes of interstitial lung diseases include idiopathic pulmonary fibrosis, sarcoidosis, hypersensitivity pneumonitis, and connective tissue diseases such as rheumatoid arthritis and systemic lupus erythematosus. Exposure to environmental factors like asbestos, silica, and certain drug-induced toxicities also contribute significantly to interstitial lung pathology. These conditions primarily affect the lung interstitium, leading to inflammation and fibrosis, which differ pathologically and radiologically from alveolar diseases characterized by airspace filling.
Clinical Manifestations: Alveolar vs Interstitial
Clinical manifestations of alveolar diseases typically include rapid onset of cough, dyspnea, and production of frothy or blood-tinged sputum, reflecting alveolar space involvement and impaired gas exchange. In contrast, interstitial lung diseases often present with progressive exertional dyspnea, a dry cough, and bibasilar crackles due to fibrosis and inflammation of the lung interstitium. Chest imaging in alveolar pathology reveals alveolar infiltrates or consolidation, whereas interstitial disease shows reticular or nodular patterns indicative of diffuse interstitial involvement.
Diagnostic Approaches for Differentiating Alveolar and Interstitial Patterns
High-resolution computed tomography (HRCT) remains the gold standard for differentiating alveolar from interstitial lung patterns, displaying ground-glass opacities and consolidations indicative of alveolar disease, while interstitial patterns typically reveal reticulation, honeycombing, and traction bronchiectasis. Bronchoalveolar lavage (BAL) aids in diagnosing alveolar conditions by identifying cellular profiles such as alveolar macrophages or neutrophils, whereas lung biopsy provides histopathological confirmation by distinguishing alveolar filling processes from interstitial fibrosis or inflammation. Pulmonary function tests (PFTs) complement imaging by showing restrictive patterns in interstitial lung diseases and may reveal normal or variable findings in alveolar disorders, thus guiding accurate diagnosis and management.
Imaging Features: Alveolar vs Interstitial Changes
Alveolar changes on imaging typically present as consolidations with air bronchograms, often appearing as patchy, dense opacities localized to the alveolar spaces. Interstitial changes manifest as reticular or nodular patterns, showing thickening of interlobular septa and a fine meshwork of lines reflecting fibrosis or inflammation in the lung interstitium. High-resolution CT scans effectively differentiate these patterns, where alveolar involvement appears as ground-glass opacities or confluent consolidations, and interstitial disease shows septal lines, honeycombing, or traction bronchiectasis.
Treatment Strategies for Alveolar and Interstitial Conditions
Treatment strategies for alveolar conditions often focus on improving gas exchange and reducing inflammation through corticosteroids, oxygen therapy, and in some cases, mechanical ventilation. Interstitial lung diseases require targeted approaches such as antifibrotic agents, immunosuppressants, and pulmonary rehabilitation to slow disease progression and enhance lung function. Both conditions benefit from early diagnosis and personalized treatment plans tailored to the severity and underlying causes.
Prognosis and Long-term Outcomes of Alveolar vs Interstitial Lung Diseases
Alveolar lung diseases generally exhibit a more acute clinical course with potential for significant recovery if timely treated, whereas interstitial lung diseases often present a chronic, progressive trajectory with variable but frequently poorer long-term outcomes. Prognosis in alveolar diseases depends on the underlying etiology, such as pneumonia or alveolar hemorrhage, and typically shows better reversibility compared to interstitial lung diseases like idiopathic pulmonary fibrosis, where fibrosis leads to irreversible lung damage and decreased survival rates. Long-term outcomes in interstitial diseases are influenced by factors including extent of lung fibrosis, response to antifibrotic therapies, and comorbid conditions, resulting in a generally guarded prognosis compared to alveolar disorders.
Alveolar Infographic
 libterm.com
libterm.com