Urethritis is an inflammation of the urethra often caused by bacterial or viral infections, leading to painful urination and increased urgency. Proper diagnosis and treatment are essential to prevent complications such as urinary tract infections or transmission to sexual partners. Discover more about symptoms, causes, and effective treatments to protect your urinary health in the rest of this article.
Table of Comparison
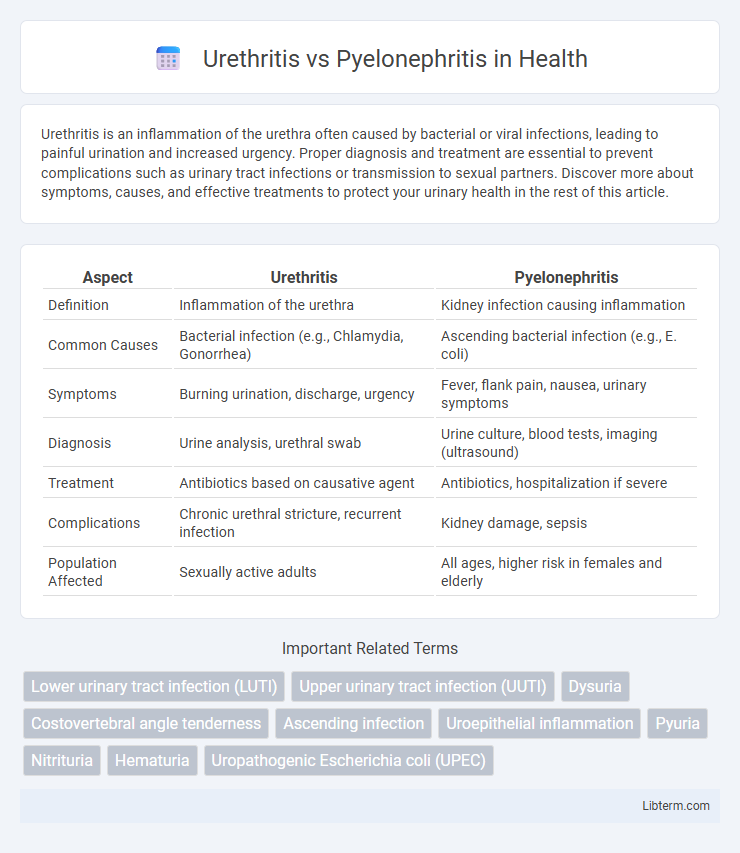
| Aspect | Urethritis | Pyelonephritis |
|---|---|---|
| Definition | Inflammation of the urethra | Kidney infection causing inflammation |
| Common Causes | Bacterial infection (e.g., Chlamydia, Gonorrhea) | Ascending bacterial infection (e.g., E. coli) |
| Symptoms | Burning urination, discharge, urgency | Fever, flank pain, nausea, urinary symptoms |
| Diagnosis | Urine analysis, urethral swab | Urine culture, blood tests, imaging (ultrasound) |
| Treatment | Antibiotics based on causative agent | Antibiotics, hospitalization if severe |
| Complications | Chronic urethral stricture, recurrent infection | Kidney damage, sepsis |
| Population Affected | Sexually active adults | All ages, higher risk in females and elderly |
Introduction to Urethritis and Pyelonephritis
Urethritis is the inflammation of the urethra, commonly caused by bacterial infections such as Neisseria gonorrhoeae and Chlamydia trachomatis, leading to symptoms like painful urination and discharge. Pyelonephritis refers to a severe kidney infection involving the renal pelvis and parenchyma, often resulting from ascending urinary tract infections caused by Escherichia coli. Both conditions require prompt diagnosis and targeted antibiotic therapy to prevent complications and preserve urinary tract function.
Key Differences Between Urethritis and Pyelonephritis
Urethritis primarily involves inflammation of the urethra caused by bacterial or viral infections, often presenting with symptoms like painful urination and discharge. Pyelonephritis is a serious kidney infection affecting the renal pelvis and parenchyma, characterized by high fever, flank pain, and systemic signs of infection. Key differences include the anatomical location, severity, and potential complications, with pyelonephritis requiring more aggressive treatment due to risk of kidney damage, whereas urethritis is generally localized and less severe.
Causes and Risk Factors
Urethritis primarily results from bacterial infections such as Neisseria gonorrhoeae and Chlamydia trachomatis, often linked to unprotected sexual activity and poor hygiene. Pyelonephritis, a severe kidney infection, commonly arises from ascending urinary tract infections caused by Escherichia coli, with risk factors including urinary obstruction, diabetes mellitus, and female anatomy. Both conditions share bacterial origins but differ significantly in their infection sites and associated predisposing factors.
Common Signs and Symptoms
Urethritis typically presents with dysuria, urethral discharge, and increased urinary frequency, primarily affecting the lower urinary tract. Pyelonephritis manifests with flank pain, high fever, chills, nausea, and costovertebral angle tenderness, indicating upper urinary tract involvement. Both conditions can cause urinary discomfort, but pyelonephritis often involves systemic symptoms and more severe illness.
Diagnostic Approaches
Urethritis diagnosis primarily involves urine analysis, including nucleic acid amplification tests (NAATs) to detect causative agents like Chlamydia trachomatis and Neisseria gonorrhoeae, alongside urethral swab cultures. Pyelonephritis diagnosis requires imaging studies such as renal ultrasound or CT scan to identify kidney involvement, combined with urinalysis showing pyuria and urine culture indicating significant bacteriuria. Blood cultures and inflammatory markers like C-reactive protein (CRP) and leukocyte count are critical in distinguishing pyelonephritis from lower urinary tract infections like urethritis.
Complications and Risks
Urethritis primarily risks complications such as chronic urethral strictures and increased susceptibility to sexually transmitted infections, potentially leading to infertility if untreated. Pyelonephritis poses severe risks including kidney abscesses, permanent renal scarring, and progression to sepsis or acute kidney injury, especially in diabetic or immunocompromised patients. Early diagnosis and targeted antimicrobial therapy are critical to prevent long-term renal damage and systemic infection complications.
Treatment Options
Urethritis treatment primarily involves antibiotics such as azithromycin or doxycycline for bacterial infections, targeting pathogens like Neisseria gonorrhoeae and Chlamydia trachomatis, with symptom management through analgesics and increased fluid intake. Pyelonephritis requires more aggressive therapy, often starting with intravenous antibiotics like ceftriaxone or fluoroquinolones for severe cases, followed by oral antibiotics once symptoms improve, addressing common causative agents including Escherichia coli. Hospitalization may be necessary for pyelonephritis patients presenting with systemic signs or complications, emphasizing the importance of prompt, tailored antimicrobial regimens to prevent renal damage.
Prevention Strategies
Effective prevention of urethritis involves maintaining proper personal hygiene, practicing safe sex by using condoms, and avoiding irritants like harsh soaps or chemicals. Pyelonephritis prevention centers on promptly treating lower urinary tract infections, ensuring adequate hydration to flush bacteria, and managing underlying conditions such as kidney stones or diabetes. Regular medical check-ups and urinary tract health monitoring reduce the risk of both urethritis and pyelonephritis complications.
When to Seek Medical Attention
Seek medical attention immediately for urethritis if you experience painful urination, frequent urges to urinate, or unusual discharge, especially if symptoms persist beyond a few days. Pyelonephritis requires prompt medical care when symptoms include high fever, chills, flank pain, nausea, or vomiting, as it indicates a kidney infection that can cause serious complications. Early diagnosis and treatment of these urinary tract infections prevent progression to severe illness and reduce the risk of kidney damage or systemic infection.
Prognosis and Long-term Outcomes
Urethritis generally has a favorable prognosis with prompt antibiotic treatment, leading to full recovery and minimal long-term complications. Pyelonephritis, particularly when severe or recurrent, can result in chronic kidney damage, hypertension, or renal scarring, posing significant risks for long-term renal impairment. Early diagnosis and effective management are critical to prevent persistent kidney dysfunction and adverse outcomes in pyelonephritis cases.
Urethritis Infographic
 libterm.com
libterm.com